new to the gluten free journey?
new to the gluten free journey?

Celiac disease is an autoimmune condition that is triggered by the ingestion of gluten. When you have celiac disease, your body perceives gluten as an invader, which causes your body to launch an immune response. This causes inflammation in the intestinal tract and other parts of the body. Systemic inflammation then contributes to further autoimmunity and health concerns. Those who have celiac disease need to avoid gluten, a type of protein found in grains.
Typically, the avoidance of gluten is enough for a person to start feeling better and for their body to start healing. But in some cases, people do not respond to a gluten free diet and continue to have symptoms. This is a form of celiac disease called refractory celiac disease.
Contents
ToggleRefractory celiac disease is a form of celiac disease that does not respond to a gluten-free diet. Refractory celiac disease is much less common than celiac disease and presents as persistent or recurrent symptoms or signs of celiac disease.
Celiac disease can cause and coexist with several other conditions. Many of these other conditions can go unrecognized after a celiac disease diagnosis. Unfortunately, the celiac disease diagnosis can mask other issues. In addition, celiac disease can cause damage to the intestines and body that must heal, even after a gluten free diet is adopted.
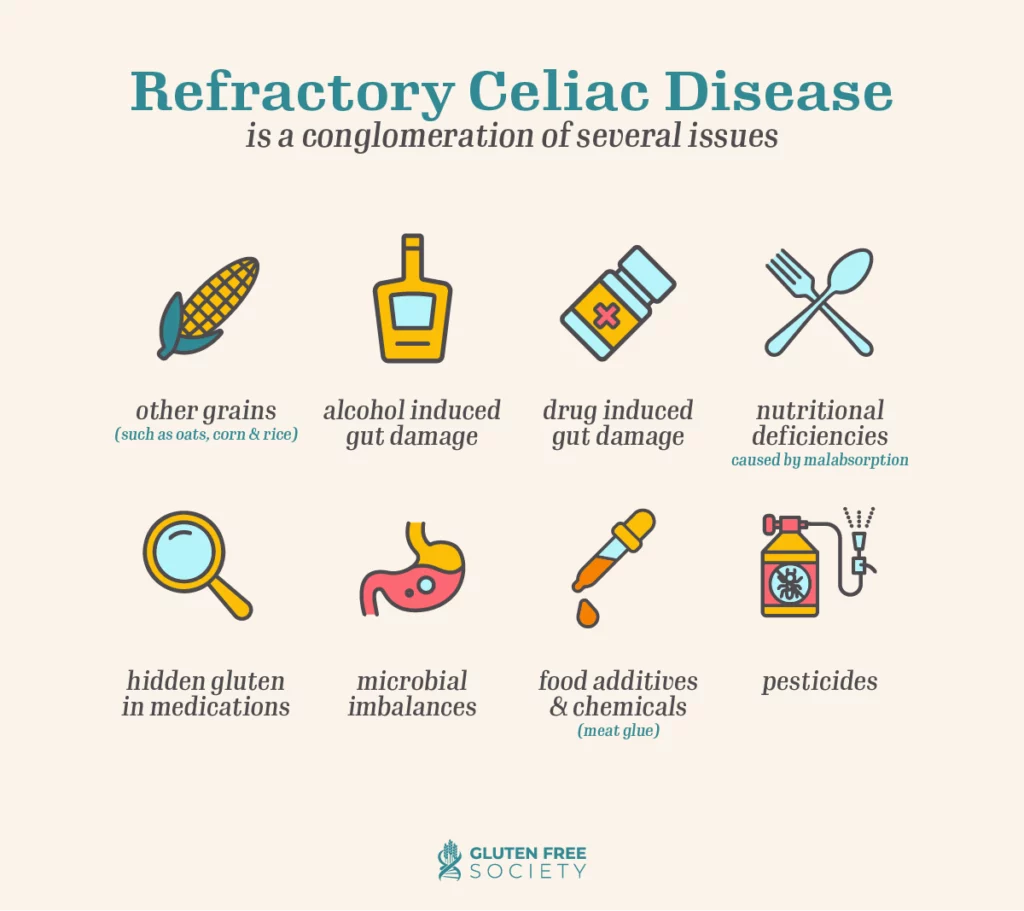
For these reasons, many practitioners and researchers, including Gluten Free Society’s Dr. Peter Osborne believe that refractory disease is actually just a conglomeration of several issues. Some of these issues include the following:
Symptoms of refractory celiac disease generally align with the symptoms of celiac disease. In some cases, they are just more severe. Common symptoms include the following:
In addition, symptoms of complications from celiac disease may show up, including the following:
Causes of refractory celiac disease are not fully understood. We know that there is a genetic component to celiac disease, which may influence the development of refractory celiac disease.
There are also environmental factors that may contribute to the development of refractory celiac disease.
Many chemicals in our environment, known as persistent organic pollutants (POPs), are considered endocrine disruptors. Research has explored the effect that POPs may have on celiac disease, given the important interplay between the endocrine and immune systems. One study found that patients with higher serum dichlorodiphenyldichloroethylene (DDE) concentrations had a two-fold higher odds of celiac disease. DDE may be found in food, water, or elsewhere in the environment.
Studies have shown that some intestinal parasites can have an effect on the immune system of their infected hosts. In fact, in some cases, they are even able to modify and change the host’s immune responses, especially in autoimmune disorders like celiac disease.
Many medications may cause a reaction similar to the small intestinal mucosal inflammatory process of celiac disease. These include alcohol, antibiotics (eg., neomycin), non-steroidal anti-inflammatory drugs (eg., sulindac), stathmokinetic and chemotherapeutic agents (eg., colchicine, vincristine, methotrexate) and immunosuppressive medications (eg., azathioprine, mycophenolate mofetil). Several newer drugs have also recently been recognized to cause a sprue-like intestinal disease. These include pharmaceuticals, such as olmesartan, an angiotensin II receptor antagonist used in the treatment of hypertension, and biologicals, specifically ipilimumab, a humanized monoclonal antibody designed to overcome cytotoxic T-lymphocyte antigen-4, used in treatment of some advanced malignancies, including malignant melanoma.
Stay up-to-date with the latest articles, tips, recipes and more.

*These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure or prevent any disease.
If you are pregnant, nursing, taking medication, or have a medical condition, consult your physician before using this product.
The entire contents of this website are based upon the opinions of Peter Osborne, unless otherwise noted. Individual articles are based upon the opinions of the respective author, who retains copyright as marked. The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Peter Osborne and his community. Peter Osborne encourages you to make your own health care decisions based upon your research and in partnership with a qualified health care professional.