new to the gluten free journey?
new to the gluten free journey?
Contents
Toggle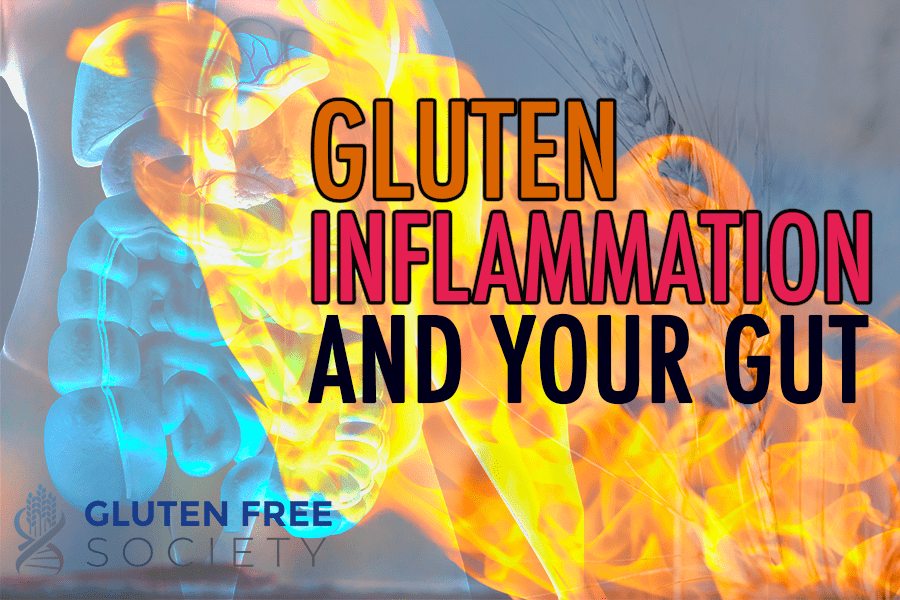 Can gluten cause gut inflammation? It is well known that gluten causes celiac disease – an inflammatory condition of the small intestine. What is less well known, and often times completely ignored, is the connection between gluten and inflammation of other areas of the GI tract. Keep in mind that the GI tract is made up of the entire tube running from your mouth to your anus. Gluten induced inflammation has been medically researched and documented in the mouth, esophagus, stomach, small intestine, and large intestine. In other words, gluten can damage any area along the GI tract.
Inflammatory bowel disease (IBD) is a broad term used to describe a variety of conditions that cause chronic inflammation in the digestive tract. Crohn’s disease and ulcerative colitis (UC) are commonly included under the IBD umbrella. But they’re not the only inflammatory bowel diseases. For example, celiac disease causes chronic gut inflammation. Others conditions include:
Can gluten cause gut inflammation? It is well known that gluten causes celiac disease – an inflammatory condition of the small intestine. What is less well known, and often times completely ignored, is the connection between gluten and inflammation of other areas of the GI tract. Keep in mind that the GI tract is made up of the entire tube running from your mouth to your anus. Gluten induced inflammation has been medically researched and documented in the mouth, esophagus, stomach, small intestine, and large intestine. In other words, gluten can damage any area along the GI tract.
Inflammatory bowel disease (IBD) is a broad term used to describe a variety of conditions that cause chronic inflammation in the digestive tract. Crohn’s disease and ulcerative colitis (UC) are commonly included under the IBD umbrella. But they’re not the only inflammatory bowel diseases. For example, celiac disease causes chronic gut inflammation. Others conditions include:
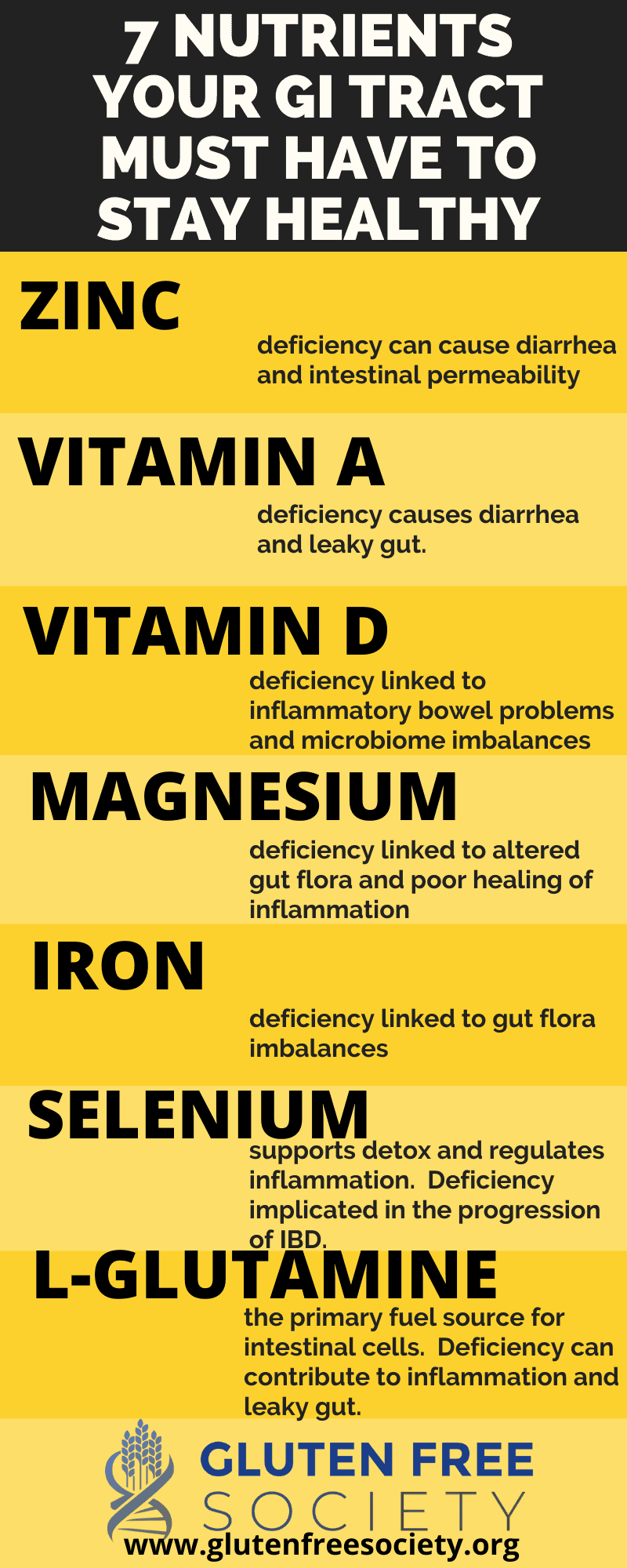
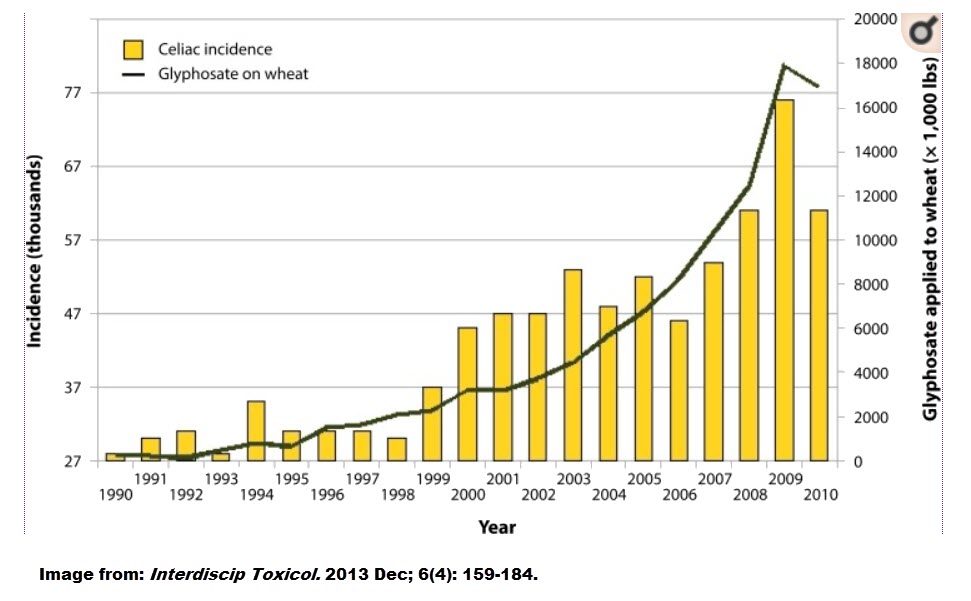 There’s also evidence that glyphosate, causes gut bacteria imbalances. It also binds to minerals (e.g., iron) and amino acids, which prevents them from getting absorbed and leads to nutrient deficiencies that can contribute to IBD.
In addition, research tells us that glyphosate significantly reduces the amount of manganese that plants absorb from the soil. Thus, eating a diet rich in processed foods is deficient in manganese. And this presents a problem because manganese is used by certain gut bacteria for a wide range of functions, which includes fighting against inflammation in the gut as well as cellular damage from free radicals.
Glyphosate may also be associated with a condition known as cholestasis, which reduces or restricts your body’s flow of bile, a condition common among patients with IBD.
Most recently, glyphosate has been linked to non-Hodgkin’s lymphoma, and cancer that can impact the digestive tract. The producer of glyphosate, Bayer, has been ordered to pay out 10 billion in damages over this connection.
There’s also evidence that glyphosate, causes gut bacteria imbalances. It also binds to minerals (e.g., iron) and amino acids, which prevents them from getting absorbed and leads to nutrient deficiencies that can contribute to IBD.
In addition, research tells us that glyphosate significantly reduces the amount of manganese that plants absorb from the soil. Thus, eating a diet rich in processed foods is deficient in manganese. And this presents a problem because manganese is used by certain gut bacteria for a wide range of functions, which includes fighting against inflammation in the gut as well as cellular damage from free radicals.
Glyphosate may also be associated with a condition known as cholestasis, which reduces or restricts your body’s flow of bile, a condition common among patients with IBD.
Most recently, glyphosate has been linked to non-Hodgkin’s lymphoma, and cancer that can impact the digestive tract. The producer of glyphosate, Bayer, has been ordered to pay out 10 billion in damages over this connection.
Stay up-to-date with the latest articles, tips, recipes and more.

*These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure or prevent any disease.
If you are pregnant, nursing, taking medication, or have a medical condition, consult your physician before using this product.
The entire contents of this website are based upon the opinions of Peter Osborne, unless otherwise noted. Individual articles are based upon the opinions of the respective author, who retains copyright as marked. The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Peter Osborne and his community. Peter Osborne encourages you to make your own health care decisions based upon your research and in partnership with a qualified health care professional.
4 Responses
I’ve been gluten free for 10 years. I still have problems with constipation and hemorrhoids. I realized I needed to go low oxalate recently because of oxalate crystals in my urine causing neuropathy and neuroma. I believe I may have leaky gut. Our bodies are so complex. I cut out all grains and many other things this summer based on your No Grain No Pain book.
I’m stumped. Maybe it takes a while for the oxalate crystals to leave my system. I cut out high oxalate foods about 3 weeks ago.
Any suggestions?
What a amazingly informative article. It has given me lot to think about and hope that my conditions can be addressed.
I got hyperthyroidism and stomach inflammation
My test came back to be Celiac Sensitive. In this article, I have no constipation, and other symptoms for celiac.