new to the gluten free journey?
new to the gluten free journey?
Contents
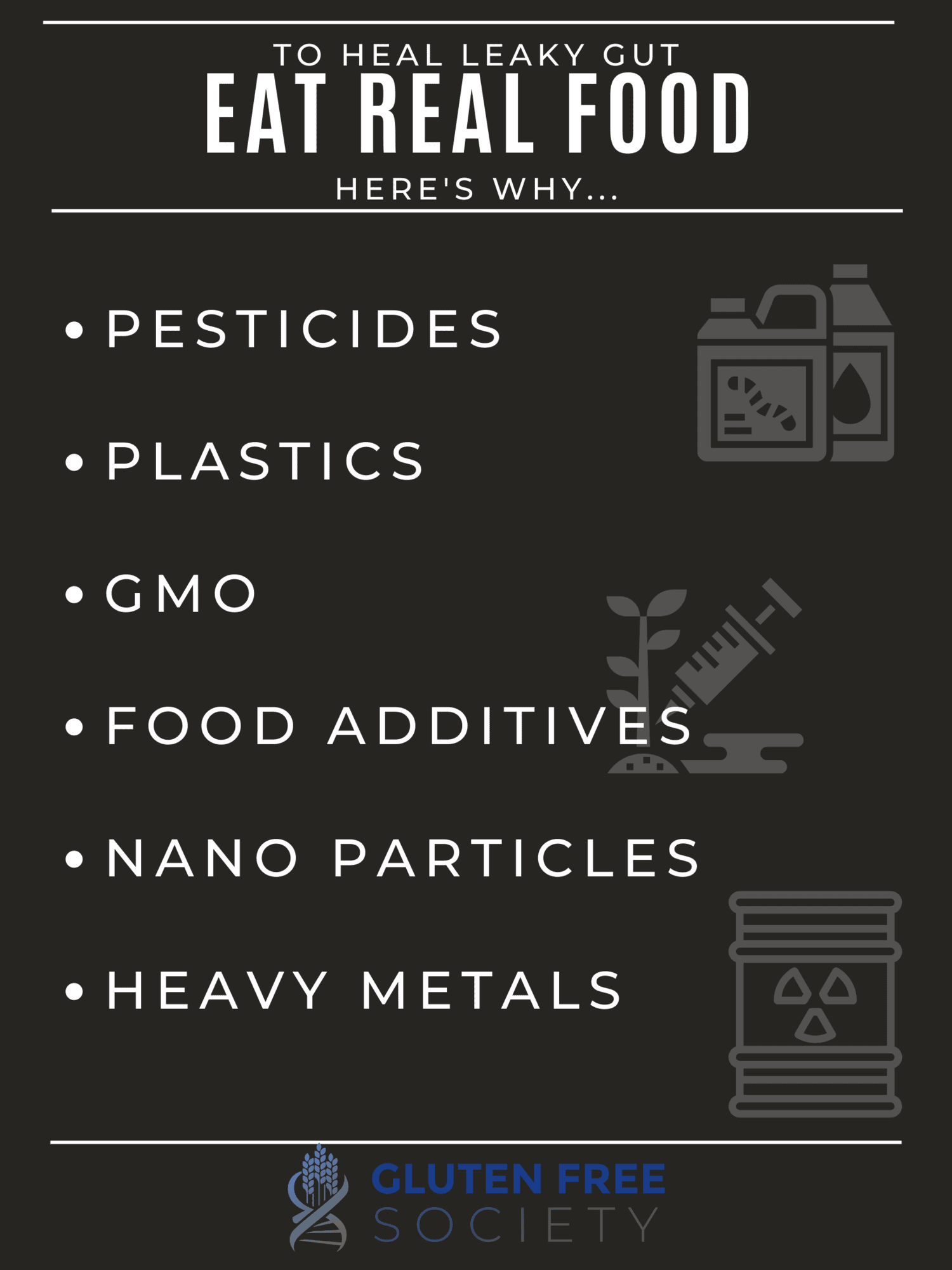
Toggle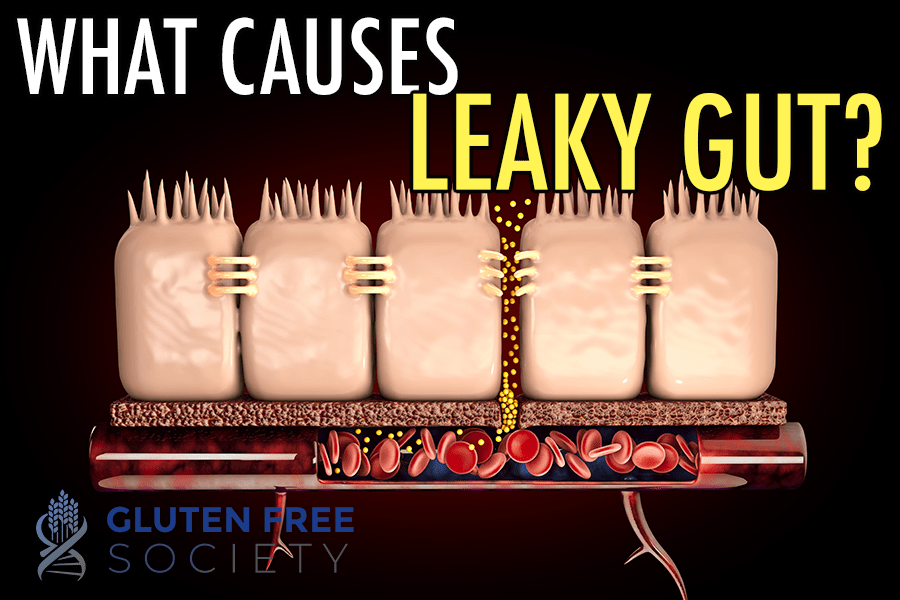 What Causes Leaky Gut – Going Beyond Gluten
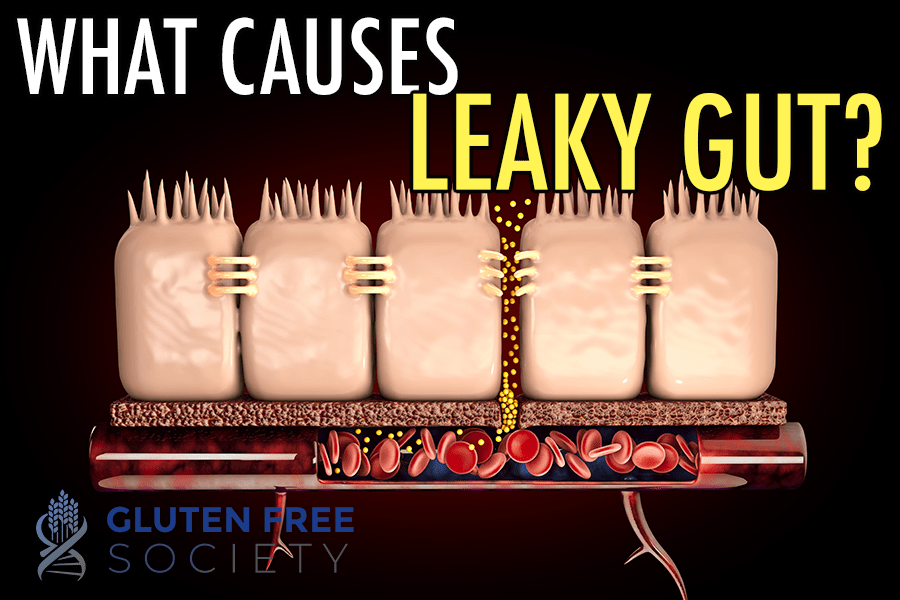
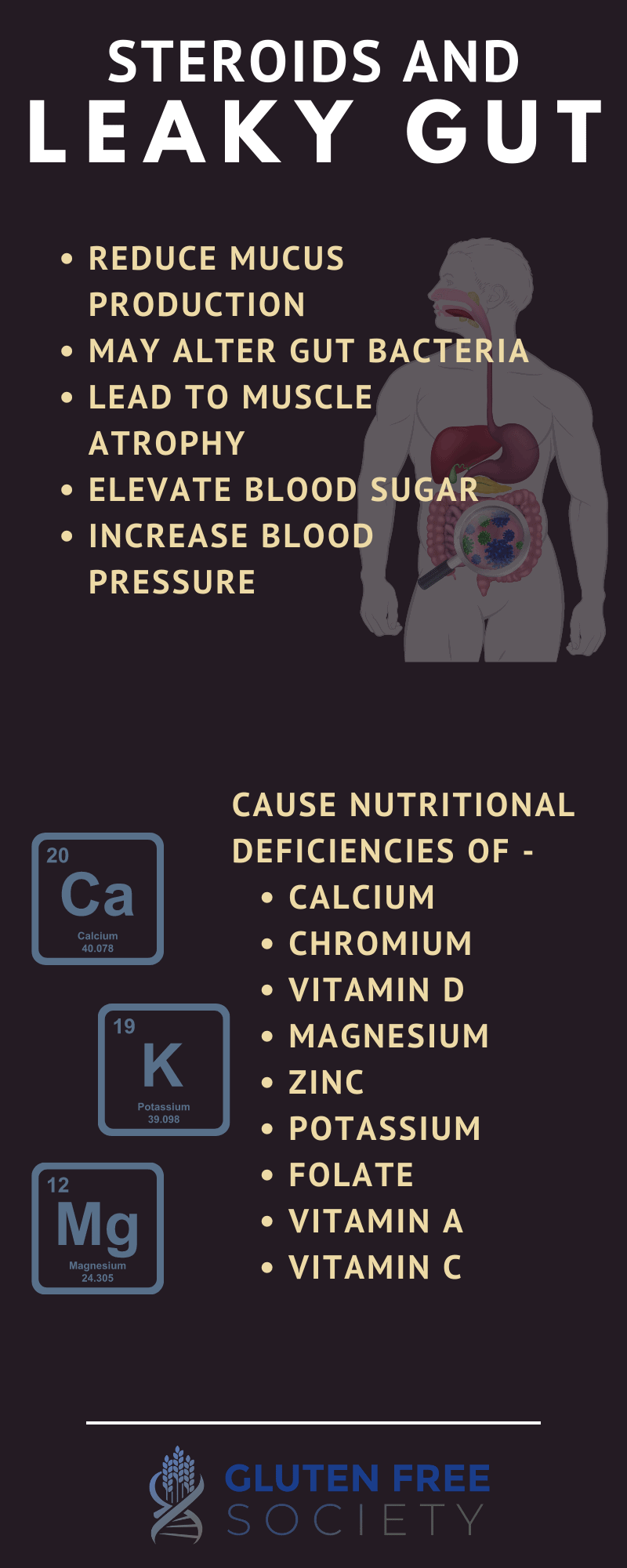
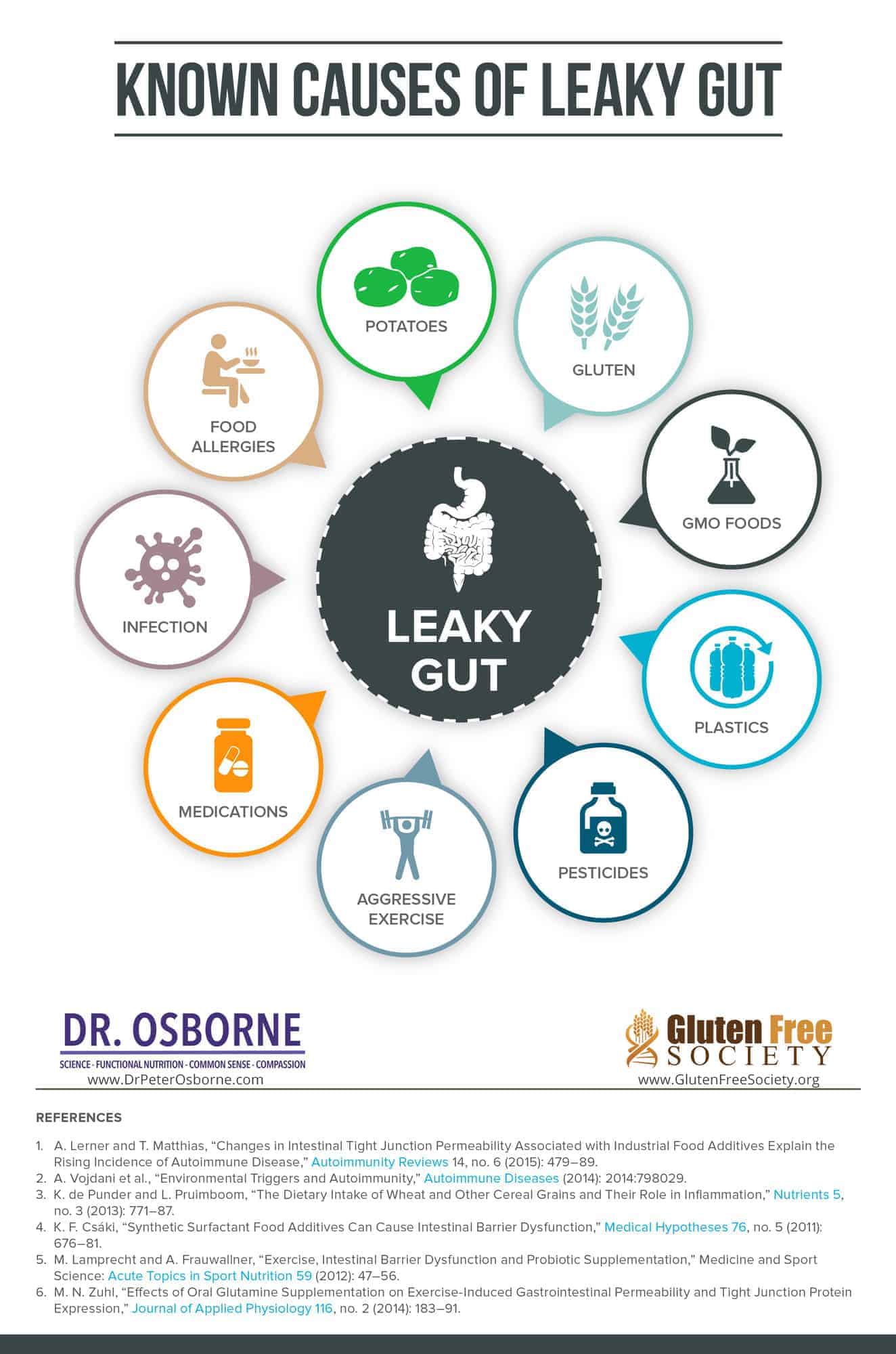
What Causes Leaky Gut – Going Beyond Gluten
 DId you overcome leaky gut? Leave your comments below…
DId you overcome leaky gut? Leave your comments below…
Stay up-to-date with the latest articles, tips, recipes and more.

*These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure or prevent any disease.
If you are pregnant, nursing, taking medication, or have a medical condition, consult your physician before using this product.
The entire contents of this website are based upon the opinions of Peter Osborne, unless otherwise noted. Individual articles are based upon the opinions of the respective author, who retains copyright as marked. The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Peter Osborne and his community. Peter Osborne encourages you to make your own health care decisions based upon your research and in partnership with a qualified health care professional.
13 Responses
Wow. That was an excellent article. Thank you, Dr.Osborne.
Educative & Informative
I’d like to see you include the effects of alcohol on the gut process.
Great information, can gluten sensitivities-or celiac cause ankylosis spondylitis
Nancy – Yes. I have seen this both in my clinic as well as reported by other researchers. Check out the following articles on the topic.
https://env-gfsociety-staging.kinsta.cloud/can-eating-gluten-cause-back-pain/
https://env-gfsociety-staging.kinsta.cloud/ankylosing-spondylitis-as-uveitis-and-asthma-resolved-on-gluten-free-diet/
All the best,
Dr. O
How long does it take to repair the gut?
I eat gluten free and none of the rx & otc pills and I take all the good vitamins you list and still have lots of gas and stomach vibration at night an have poor sleep. Have not found an answer.
I take digest enzymes before meals. Can’t find help for myself anywhere.
You have to go 100% grain-free. A gluten-free product may still contain grains like rice and corn, oats etc… I had this experience. Avoid all grains and nightshades and dairy for 30 days and see how you feel 30 days later— to start. Dr. O’s site is a wealth of info. Research leaky guy healing diet for food ideas to start step by step. I’m grateful for all the help I’ve found here. Life-saving! I feel like a 5 year old and should be retiring now but have all this energy and zest for life, so stay active with work projs and creatives. You’ll feel the difference too. xx
Great explained information, thank you Dr.Osborne,
How much time does it need to heal the gut ?
Also I have a gum infection, does that trigger the gut as well?
Excellent article, very informative!
Thank you
I have a gut feeling about the science of gut, though I’ve never been scientifically minded. I am a student of Dr. Osborn’s podcast.
It was a fantastic article!. I am learning so much. I wish I had known all of these when I was younger. I am passing what I am learning to whoever wants to listen. Thank you, Dr. Osborne.
YES, U HEALED ME WITH UR KNOWLEDGE. I AM 61 YRS OLD & DIAGNOSED WITH RA THAT ALMOST CRIPLED ME WITHIN 1 YEAR . YOUR VIDEO POPPED UP ON MY UTUBE OF YPU ADDRESSING A BOARD THAT YOU HAD A CURE. I WAS SENSITIVE TO EGGS.. I REMOVED THEM AND WITHIN DAYS NY INFLAMMATION THROUGHOUT BODY DECREASED DAILY. IM 90% BETTER … I’M SO GRATEFUL… GOD BLESS YOU.