new to the gluten free journey?
new to the gluten free journey?

Can gluten cause headaches? This simple answer is yes. I bet it’s safe to say that you’ve experienced a headache or two in your lifetime. Maybe even more. Because headaches are one of the most commonly reported medical complaints. And they can range from a dull ache to debilitating pain.
Headaches are most often treated with pain killers and other prescription medications. However, these treatments don’t address the underlying problem. They don’t eliminate your triggers. Plus, there’s a risk of addiction as well as other serious side effects.
The fact is your diet and lifestyle influence every aspect of your physical and emotional health. And there’s undeniable evidence that gluten is associated with a long list of symptoms, abnormalities, and diseases. So it’s not surprising that gluten may also trigger headaches.
There are several types of headaches defined in the medical community. In this article, I’ll discuss how gluten can contribute to migraines as well as cluster and tension headaches.
Contents
ToggleMigraines are the 3rd most prevalent disease and the 6th leading cause of disability worldwide. The pain ranges from moderate to severe and typically lasts for 4 to 72 hours.
In many cases (but not all), migraines occur on one side of the head. You may also experience:
Plus, any movement can make things worse. This is why many sufferers often lie in a dark, quiet room and remain there until the migraine passes.
Some people develop chronic migraines. They spend more than half their days in pain. Many never find permanent relief. Because most triggers are overlooked.
Triggers for migraines may be genetic or hormonal. But they may also be environmental, including food and chemicals in our food, cleaning products, and cosmetics. Plus, environmental factors can influence our genetics and hormones creating a vicious cycle.
Based on my professional experience, I’m certain that gluten is a migraine trigger for some. And there’s plenty of scientific evidence to support my findings.
A recent meta-analysis looked at 40 scientific studies published since 1987 that discussed the connection between headaches and celiac disease. From the data, they determined that the prevalence of headaches (mostly migraines) among those with celiac disease was 26% for adults and 18.3% for children. However, the prevalence of migraines among the general population including both adults and children is only 12%. Thus, these numbers suggest that migraines affect those with celiac disease more frequently than those without.
In this study, researchers found that those with celiac disease were 4 times more likely to experience migraine headaches than a control group. While migraines didn’t last as long as the control group, they occurred 2.5 times more frequently than those without celiac disease. When put on a gluten-free diet, migraines disappeared in 25% of the celiac patients. And 38% experienced a reduction in the severity and frequency of their headaches.
Numerous case studies suggest that migraines of unknown origin (a.k.a. idiopathic) may be one of the first symptoms of celiac disease.
In a study of 48 school-aged children with celiac, neurological symptoms were the first sign of disease among 33% of them. Migraine headaches were the most frequently reported symptom. All of the children in the study were put on a gluten-free diet. Migraines and epilepsy were the two neurological symptoms that responded favorably to the diet.
A woman in this case study was diagnosed with celiac disease only after visiting her doctor due to migraine attacks that involved neurological impairments. Once placed on a gluten-free diet, her severe migraines never returned. A similar experience was reported in this case.
Another case study involved a young woman in her early twenties who presented with chronic migraines along with hives, joint pain, and missed periods. All neurological and hormonal tests performed could not explain the symptoms she was experiencing. The only clue was a potential gluten sensitivity picked up by a skin prick test. So she was placed on a gluten-free diet and her symptoms disappeared.
The doctors then challenged her system with gluten to further test their hypothesis that gluten was the cause of her symptoms. Not surprisingly, the woman broke out in hives within 20 minutes, and she had a severe headache the following day.
In some cases, migraines can be caused by the build-up of calcium in the brain known as cerebral calcification. A folate deficiency is believed to contribute to this condition. Interestingly, folate deficiencies are common among those with gluten sensitivity due to gut inflammation and subsequent malabsorption.
In this case study, a CT scan revealed cerebral calcification in the brain of a 36-year-old woman. An MRI scan ruled out Sturge-Weber syndrome and other common causes of cerebral calcification. However, blood tests revealed the presence of anti-gluten antibodies as well as low folate levels. An intestinal biopsy confirmed a celiac disease diagnosis. So the woman was put on a gluten-free diet and her neurological symptoms disappeared.
There’s also evidence that a carnitine deficiency caused by gluten-induced malabsorption can contribute to neurological symptoms. In this case study, a gentleman found himself at the hospital after he started experiencing a range of neurological symptoms, including chronic headaches. Even though he had previous signs of celiac disease, such as extreme weight loss and anemia, he was never tested.
Celiac disease was eventually confirmed as well as low carnitine levels. The patient was put on a gluten-free diet and prescribed high doses of replacement carnitine. Within two weeks, his neurological symptoms subsided and he remained symptom-free during a two year follow-up period.
Other nutrient deficiencies linked to gluten sensitivity may also be contributing factors. For example, vitamin D deficiency is a common denominator of both gluten sensitivity and migraines. According to this review, studies reported 45 – 100% of patients with migraines had low vitamin D levels.
Headaches are also a symptom of anemia, which is caused by low iron.
Plus, there’s evidence that supplementing with magnesium, carnitine, vitamins B2, B3, and B12, CoQ10, and vitamin D can help prevent and tame migraines.
However, if gluten is causing your nutrient deficiencies, supplementing isn’t enough. Eliminating gluten from your diet is a must to achieve permanent relief.
It’s worth noting that steroid shots that are sometimes used to treat migraines can deplete your body of magnesium and interfere with vitamin D activity. So while they may provide temporary relief, they may also be contributing to a never-ending cycle of migraines.

Brain scans of patients with celiac disease and migraines reveal relatively high percentages of brain abnormalities, particularly in the white matter. (White matter is found in the deepest layers of your brain and it contains many nerve fibers. It’s believed to play a role in learning, memory, and relaying messages to other parts of the brain.)
Out of 40 patients with celiac disease or gluten sensitivity in this study, 10 were found to have white matter abnormalities. All 10 experienced migraine-like headaches. And 9 out of 10 eliminated their headaches with a gluten-free diet.
For a long time, migraines were considered to be a vascular disorder in many cases. The pain was believed to be caused by abnormal dilation of blood vessels within the skull leading to the excitation of nerve fibers. However, this theory was never scientifically proven.
While research is still underway, there’s a current focus on inflammation. This new theory suggests that inflammatory compounds released in the brain may activate pain receptors and make them more sensitive to subsequent stimuli. The receptors then overreact and trigger a cascade of events that ultimately causes pain.
What causes the inflammatory agents to be released in the brain may vary among people. We know for sure that gluten can cause the release of inflammatory compounds throughout the body due to an overactive immune response, nutrient deficiencies, or a combination of both.
Gluten-induced Inflammation is also a form of stress that can stimulate the secretion of cortisol, a stress hormone. Elevated cortisol can further increase intestinal permeability and alter your gut bacteria. This may help explain why people with celiac disease tend to have gut bacteria imbalances (a.k.a. dysbiosis), including more pathogenic bacteria than healthy subjects.
Gut bacteria imbalances alone can also cause inflammation and keep your body’s stress response activated. This creates a chronic state of inflammation, which makes your body more susceptible to disease.
In addition to inflammation, gut bacteria imbalances may cause a rise in certain neurotransmitters that inhibit the secretion of stomach acid, delay stomach emptying, and reduce hunger, which can all lead to nutrient deficiencies.
Finally, certain gut bacteria are necessary to produce short-chain fatty acids, which are believed to have an anti-inflammatory effect on the brain. Thus, gut bacteria imbalances could reduce the production of short-chain fatty acids and leave the brain more susceptible to inflammation.
In addition to the inflammatory pathways discussed above, there’s evidence that pain associated with migraines in some cases may be caused by a lack of energy in the brain or oxidative stress.
Oxidative stress is caused by a build-up of free radicals. And these free radicals can come from within. But they’re also present in our environment, such as processed foods made with grains.
In addition, oxidative stress is prevented by antioxidants, such as vitamins A, C, and E as well as zinc and selenium. This is another way gluten-induced nutrient deficiencies may contribute to migraines.
A ketogenic diet is low in carbs and high in fat. Thus, it’s usually grain-free, which means it’s also gluten-free. And research supporting the use of ketogenic diets to treat migraines is promising.
Eating a ketogenic diet causes your body to switch from burning carbohydrates to burning fat. Eventually, excess fats are converted into ketone bodies. This process is called ketosis.
The brain can’t burn fat for fuel. But in the absence of glucose, it can burn ketone bodies efficiently, which can help prevent energy deficits. However, there’s evidence that ketones are more than just brain fuel. Research suggests they may also help reduce inflammation and oxidative stress in the brain, promote a healthy gut microbiome, and prevent the brain from overreacting to stimuli. All potential benefits for those who suffer from headaches.
Migraine headaches are more common among women. Plus, in over 50% of these cases, migraines are associated with menstruation due to hormonal changes.
However, while menstrual migraines may be common, they’re not normal. It’s likely a sign of an imbalance, which can be caused by many things, including gluten. In this article, I discuss several ways in which gluten can contribute to hormonal imbalances, including nutrient deficiencies and endocrine disruption.
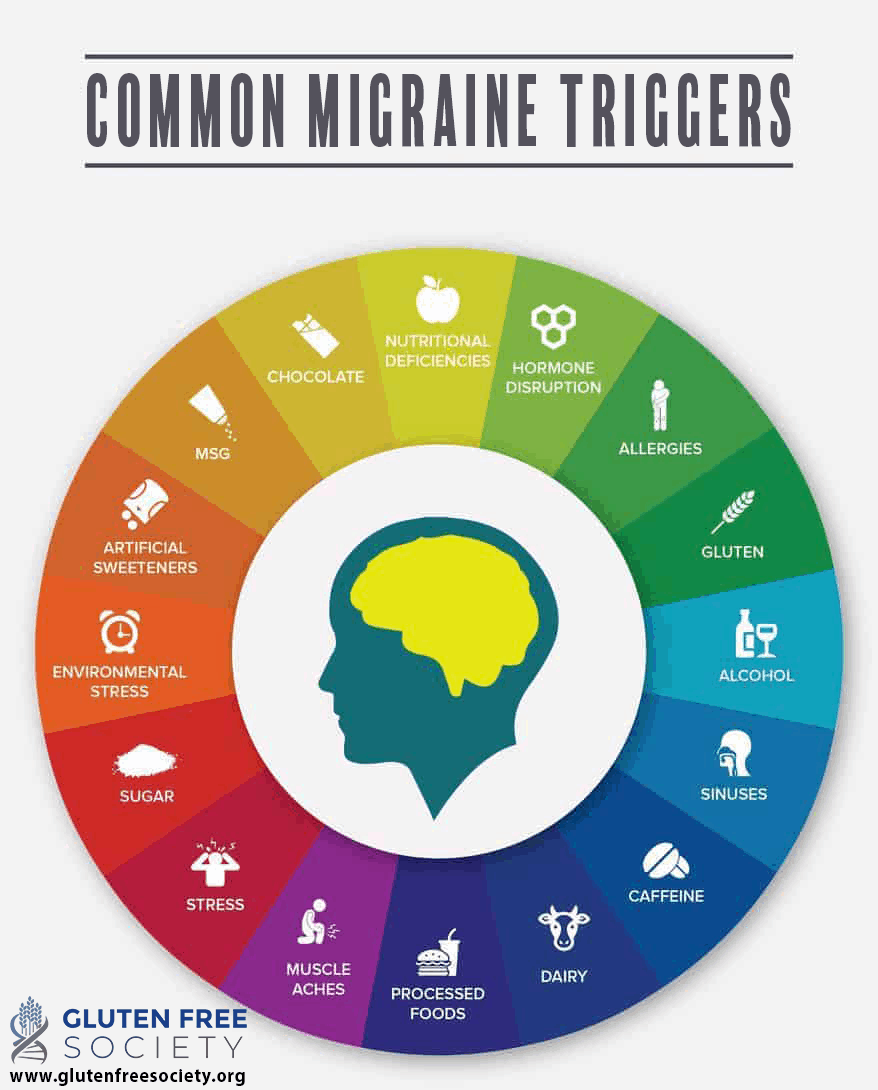
Gluten is not the only trigger for migraine headaches. The issue can definitely be multi-factorial. If you struggle with migraines, the diagram below shows a number of additional triggers you should be aware of. You can also watch this comprehensive video on the topic for more information.
Cluster headaches occur in clusters, meaning a streak of headaches followed by a normal state. They usually happen suddenly with extreme pain on one side of the head around or behind the eye that can radiate out to other parts.
Cluster headaches may be accompanied by other involuntary symptoms, such as tears, bloodshot eyes, a runny nose, and sensitivity to light. Due to the intense pain, many patients report a sense of restlessness and agitation, which causes them to pace as opposed to lay still and rest.
Unlike migraines, cluster headaches usually only last a few hours, they’re not nearly as prevalent (about 0.1% of the population), and they’re more common in men than women. Plus, the pain is often more severe than a migraine.
Like migraines, the pathways leading to the onset of cluster headaches aren’t fully understood. One of the most widely accepted theories involves the hypothalamus in your brain.
Your hypothalamus is physically connected to the vascular system that supplies nerves to the blood vessels in your brain. It’s also linked to your parasympathetic nervous system which helps your body relax and digest your food as well as perform other involuntary actions.
So it’s proposed that abnormalities in the hypothalamus or dysfunctional signaling related to the hypothalamus are responsible for causing pain as well as involuntary symptoms. To support this theory, brain scans show activity in the hypothalamus during cluster headache attacks.
Also, since the hypothalamus controls your circadian clock, this helps explain why most attacks occur around the same time shortly after falling asleep.
Another theory suggests that inflammation within the sinuses may cause damage to nerves within the skull.
So how does gluten factor in? Let’s take a look at some possibilities…
As I mentioned previously, gluten can cause inflammation throughout the body. And this includes within the hypothalamus and the sinuses.
Gluten-containing foods are also high in calories and carbohydrates. And there’s evidence that eating excess calories or high-carb diets can induce inflammation in the hypothalamus. Studies have even shown that animals can develop hypothalamic inflammation within hours of being overfed. Essentially, over-nutrition activates pathways that can cause inflammatory genes in the hypothalamus to be turned on.
This might explain why some with cluster headaches benefit from a ketogenic diet. In this study, 12 patients with cluster headaches who weren’t responding to conventional treatments were put on a ketogenic diet for three months. 75% of their calories came from fat with the remaining 25% from protein and carbohydrates.
Ten out of 12 patients responded favorably to the diet. Most within the first month. By the end of three months, seven patients were symptom-free. And three patients were only having “shadow” attacks. The researchers proposed that the benefits observed may be due to reduced inflammation and/or excitability in the brain.
Another study reported similar results. Patients were given no more than 10 grams of carbohydrates a day for 3 months. Plus, no grains were allowed. Fifteen out of 18 patients with cluster headaches found relief with a ketogenic diet. Attacks disappeared completely in 11 patients and decreased by at least 50% in the remaining four.
There’s evidence that histamine, a compound released in response to an injury or allergen, may play a role in cluster headaches. For example, in this study, histamine levels were significantly elevated in patients during a cluster headache attack.
This is relevant because elevated histamine levels are also associated with celiac disease and may even contribute to gut permeability (a.k.a. leaky gut).
In addition, gut bacteria imbalances caused by gluten may raise histamine levels. And medications often used to treat digestive symptoms commonly associated with gluten sensitivity may disrupt your gut bacteria as well as prevent histamine from being broken down and eliminated from the body efficiently.
Tension headaches are more common, but less severe than migraines and cluster headaches. They usually occur on both sides of the head and patients say it feels more like a pressing or tightening than a piercing pain.
Tension headaches are generally believed to be caused by the tensing of muscles in the head. Possibly triggered by stress, eye strain, poor posture, dehydration, and lack of sleep among other things.
If conditions aren’t addressed, the constant muscle tension may alter pain receptors in the brain, making them more sensitive and likely to cause chronic tension headaches.
There isn’t much research directly linking gluten and tension headaches, but many of my clients with gluten sensitivity experience them before going on a gluten-free diet. Research has revealed this too.
Gluten is also well-known for causing muscle pain, which I discuss in detail here. And gluten-induced magnesium deficiency can cause muscle stiffness that may contribute to tension headaches. Because magnesium is necessary for muscle relaxation.
Gluten and the damage it causes also can create physical stress as I’ve mentioned above. This puts your body in a “fight or flight” mode. And your muscles tense up during this time to give your body the strength to overcome danger.
It’s safe to say there are several ways that gluten can cause headaches directly and indirectly. Which is a really important fact for headache sufferers and doctors to understand. Because many people experience chronic, debilitating pain from headaches with no relief from conventional treatments. Common medical treatments also come with serious risks and may even make things worse.
So if you suffer from headaches and you’ve been unable to pinpoint the underlying cause, talk to an experienced doctor about your diet and nutritional status. Get screened for gluten sensitivity. Because a gluten-free diet may be the permanent solution you’ve been looking for.
Did going gluten free resolve your headaches? Share your story by commenting below.
Stay up-to-date with the latest articles, tips, recipes and more.

*These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure or prevent any disease.
If you are pregnant, nursing, taking medication, or have a medical condition, consult your physician before using this product.
The entire contents of this website are based upon the opinions of Peter Osborne, unless otherwise noted. Individual articles are based upon the opinions of the respective author, who retains copyright as marked. The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Peter Osborne and his community. Peter Osborne encourages you to make your own health care decisions based upon your research and in partnership with a qualified health care professional.
2 Responses
I have previously suffered with sinusitis and migraines. Since going gluten free a few years ago the headaches and sinus problems went away. I gradually started to be lax about my diet and started to eat gluten in bread, cakes etc. I have recently suffered the most horrible sinusitis attack which my doctor gave me 2 lots of antibiotics to try to sort. I have restarted the strictness of my no gluten regime and the headache is abating, slowly but surely.
I’m confident that gluten causes me sinus problems and migraines.
I get what I can only guess is a “tension” headaches after eating gluten. It feels like my typical headache from stress or dehydration (lack of caffeine when I used to drink coffee), frontal lobe area, achy and pulsing a little, relieved by laying down on a neck pillow (a PT told me once that there is a muscle where the neck and head meet that is nicknamed “the headache maker”). Outside of when I was dealing with BPPV, I have to say I hardly get headaches since quitting gluten. I do get ocular migraines though, here and there, but I never necessarily link that to gluten per se. I still get them, albeit far less severe and less often. I can only think, perhaps, that gluten really did influence my ocular migraines and that could be why they are less often and less severe? Either way, I’ll take it…and sticking with a gluten free diet for sure!