Eating Oxalates on a Gluten Free Diet – Is It Safe?
High oxalates on a gluten free diet might be the mistake that holds your progress back. Do you ever feel like you’re doing everything “right,” but you’re still not feeling your best? Maybe you’ve given up grains, but your symptoms still persist? Or maybe you’ve started experiencing new symptoms?
If your answer is “yes,” then I suggest learning more about oxalates. Because for some, a gluten-free or grain-free diet isn’t enough. Prefer watching a video to learn? Watch
Oxalates and Gluten here.
What are oxalates?
Oxalates are natural compounds found in both plants and humans.
Plants use vitamin C to make oxalic acid, which can bind with calcium to form calcium oxalate crystals.
Scientists believe these crystals help protect plants from calcium excess, insects, and infections as well as provide structure.
As humans, we get oxalates from eating plants that make them. Our bodies produce them under certain circumstances as metabolic by-products. And yeast and fungal infections can also contribute to the production oxalates.
However, in humans, oxalic acid and oxalate crystals are not beneficial. For perspective, oxalic acid is capable of removing rust from metal and is used commercially for this purpose. Anti-freeze (a.k.a. ethylene glycol) gets converted to oxalate in humans, which is why it’s toxic if consumed.
It’s also worth noting that deaths have been reported from the consumption of
4 – 5 grams of oxalates in food, although
10 – 15 grams are generally required to cause a fatality. But don’t worry! It’s not easy or common to consume such a high amount of oxalates at once. For reference, you’d have to eat at least 14 cups of spinach at one sitting to get to 4 grams. And over 30 cups to consume 10 grams.
Potential Effects of Oxalates in Humans
If your nutritional status is optimal, you eat a diet with lots of variety, and all systems are working as they should, oxalates in moderate doses aren’t likely to pose much of a threat. However, in today’s world, the average diet is nutrient deficient. And chronic disease is rampant. So under these conditions, oxalates shouldn’t be ignored.
Mineral Deficiencies
Oxalates can cause mineral deficiencies–in two ways. Oxalic acid can bind with minerals in your gut after a meal and prevent them from being absorbed. Oxalic acid can also be absorbed into your bloodstream and bind with minerals in circulation, which renders them useless.
When oxalic acid binds with sodium, potassium, and iron, it forms soluble salts, which can more easily be excreted from the body. When it binds to other minerals, it creates insoluble crystals that are hard to get rid of.
However, oxalic acid is most attracted to
calcium. For example, kidney stones are primarily calcium oxalate crystals.
Thus,
calcium deficiencies are common in those with oxalate issues, which can cause muscle spasms, cramps, and fatigue as well as pain, brain fog, and irritability.
Magnesium is another mineral of concern. And like calcium, magnesium deficiencies affect the muscles. They’re also associated with fatigue, high blood pressure, depression, heart problems, irritable bowel syndrome (IBS), and extreme PMS symptoms.
It’s also worth noting that magnesium deficiencies in
animal studies have been shown to contribute to the accumulation of a compound called glyoxylate. And glyoxylate can be converted to oxalate in both rodents and humans.
Kidney Disease
Your kidneys are responsible for filtering oxalates from the blood and excreting them in your urine. So
kidney disease and
stones are high risks when excess oxalates are present.
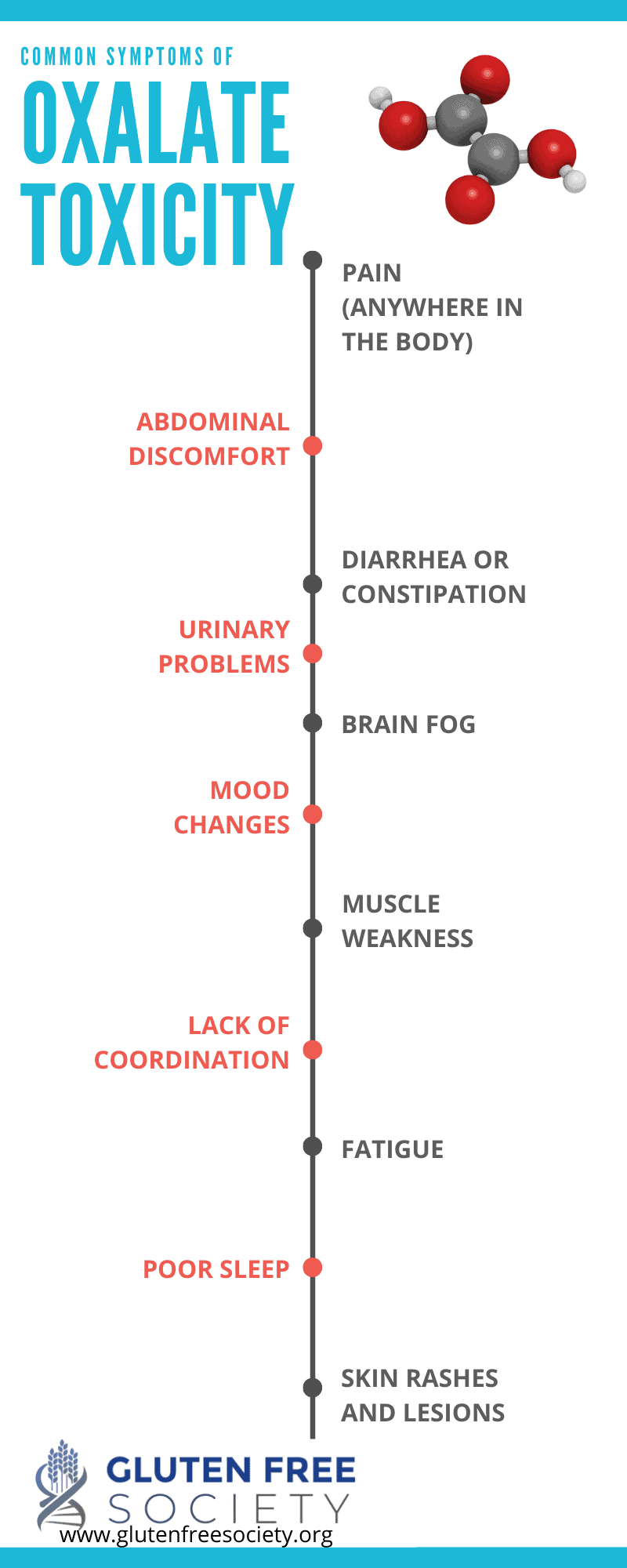
Whole-Body Effects and Symptoms
Your kidneys aren’t the only place oxalates can cause harm in your body. Oxalates are also believed to affect your
heart, thyroid, skin, joints, bones, teeth, nerves, and eyes. Essentially, crystals can damage these tissues and cause inflammation, dysfunction, and disease.
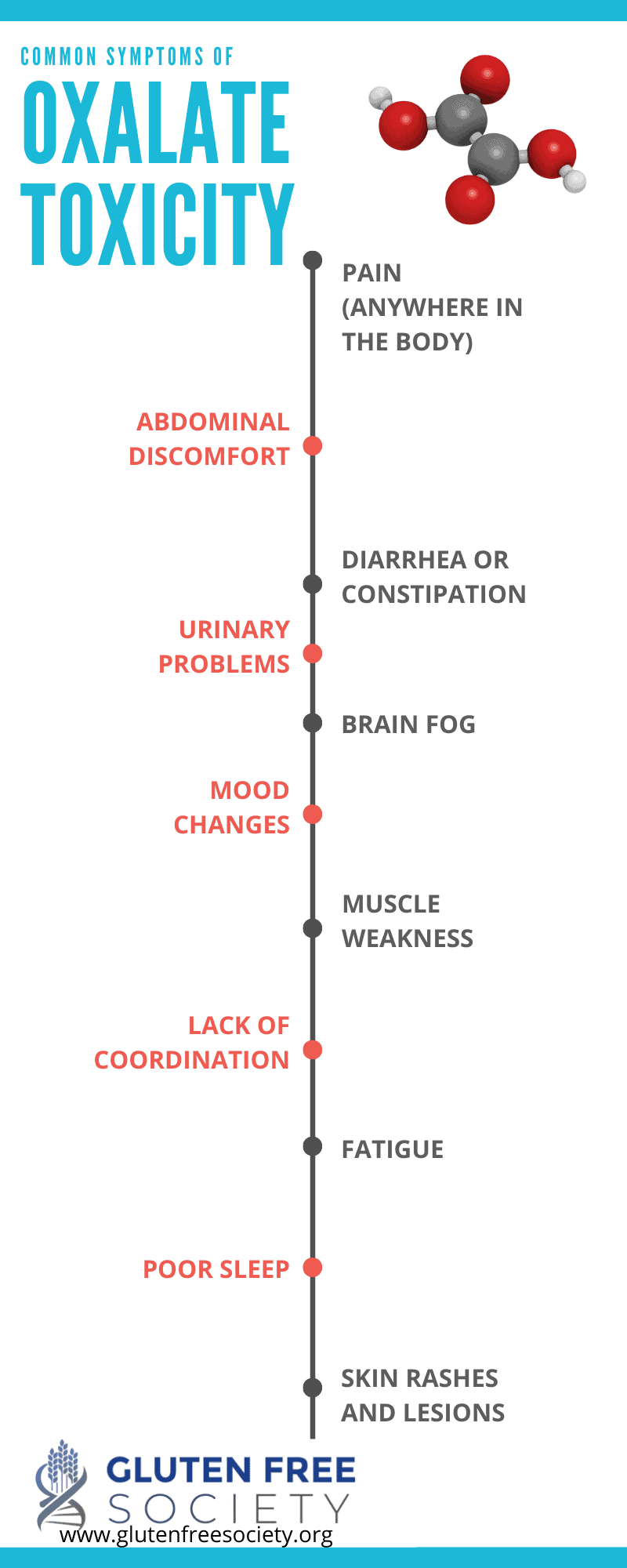
Thus, oxalate-related symptoms are broad, and may include:
- Pain (anywhere in the body)
- Abdominal discomfort
- Diarrhea or constipation
- Urinary problems
- Brain fog
- Mood changes
- Muscle weakness
- Lack of coordination
- Fatigue
- Poor sleep
- Skin rashes and lesions
- Slow healing injuries
Diseases Linked to Oxalates
Because oxalates can affect most tissues in your body, an excess is associated with many chronic disorders, including:
Plus,
experts believe that oxalates may be the missing link for those with celiac disease that don’t find relief with a gluten-free diet.
Grains, Gluten, and Oxalates
There’s more than one connection when it comes to gluten and oxalates. So let’s take a look…
Grains are High Oxalate Foods
The first point I want to make is that grains, the source of gluten, are generally high in oxalates. This is especially true for wheat, bulgar, barley, rye, brown rice, and teff. The pseudograins buckwheat, amaranth, and quinoa are also high in oxalates.
In addition,
oxalates concentrate most in the bran, the outer layer of the grain. So whole grains have higher amounts of oxalates when compared to refined grains, such as white flour and white rice.
Grain Induced Inflammation
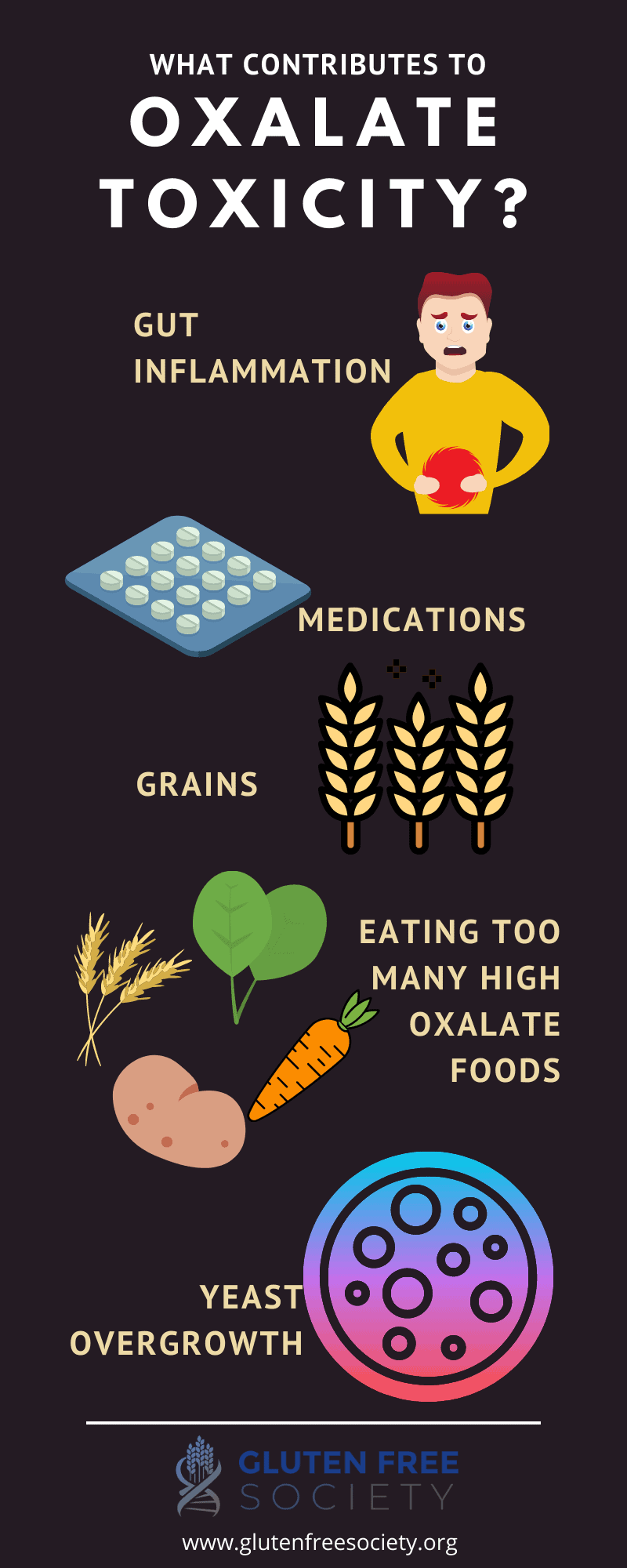
For some, gluten damages the lining of the intestines and causes
inflammation. As a direct result,
more oxalates are absorbed into the bloodstream. In addition, gut dysfunction may make it
harder to eliminate accumulated oxalates.
Grain Induced Malabsorption
Intestinal inflammation also disrupts the digestive process and prevents certain nutrients from being absorbed.
Fat is one example. And when fat malabsorption occurs,
more oxalates may enter the body. Essentially,
fat can bind to calcium, which then prevents calcium from binding to oxalates in the gut and being eliminated in your bowels.
This specific condition involving fat malabsorption, known as enteric hyperoxaluria, is also associated with
irritable bowel disease, chronic pancreatitis, bariatric surgery, and celiac disease.
Vitamin B6 deficiency is common in those with gluten sensitivity. This stems from intestinal damage as well as the fact that a grain-rich diet doesn’t provide an adequate supply of vitamin B6. This is problematic because when vitamin B6 levels are low, your body is more likely to
convert certain compounds (e.g., the amino acid glycine) into oxalate.
Gut Bacteria Imbalances Induced By Gluten and Grains
Gluten, pesticides (e.g., glyphosate), additives in processed foods, and intestinal damage from gluten can all disrupt the balance of bacteria residing in your gut. More specifically, it can
reduce species of bacteria (e.g., oxalobacter formigenes) that are capable of degrading oxalates, which help prevent oxalate absorption as well as help eliminate oxalates from the body.
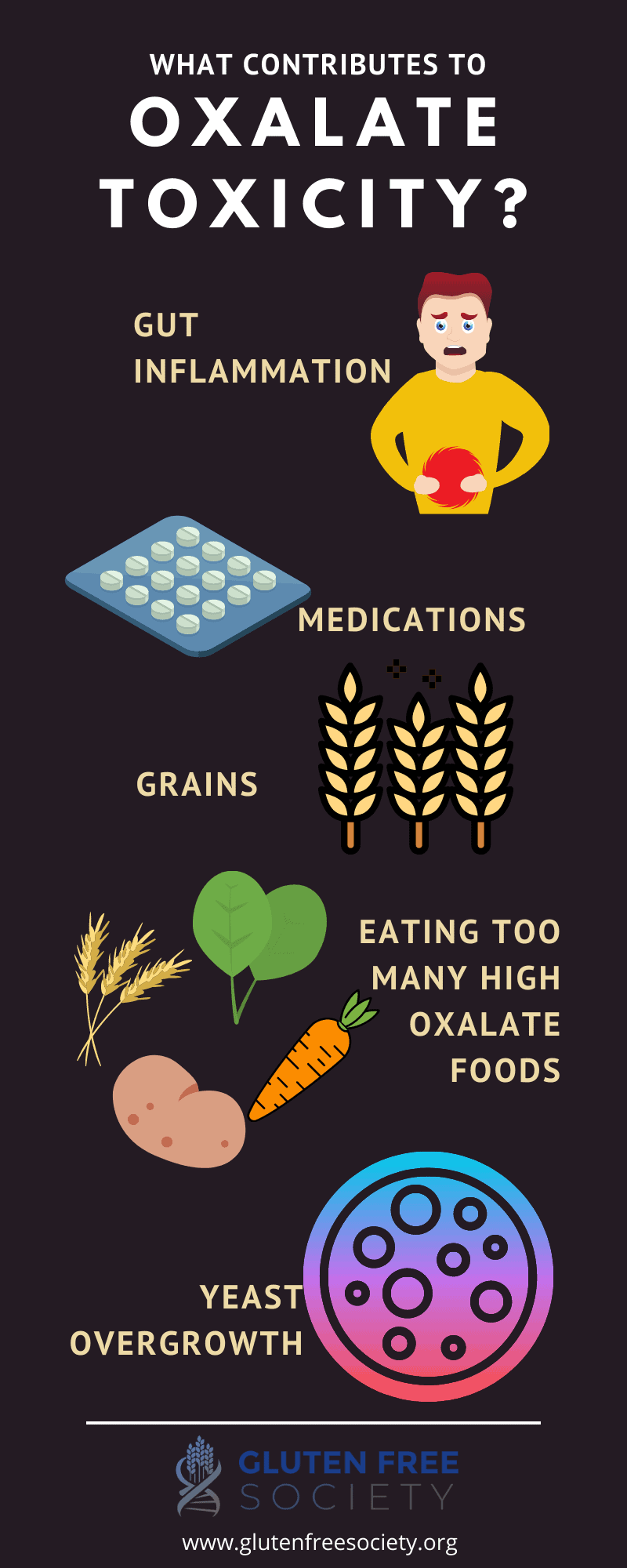
Yeast Infections
Eating a gluten-rich, processed food diet is also
associated with candida (i.e., yeast) infections. Candida produces an enzyme capable of breaking down collagen in your body. And the by-products of this reaction can be
converted into oxalates.
Medications to Treat Gluten Related Symptoms
Those with gluten sensitivity may be treated with medications that can increase the burden of oxalates. For example, NSAIDs can damage the lining of your gut as well as your kidneys. Steroids can also cause intestinal harm. And
antibiotics can kill beneficial gut bacteria that degrade oxalates.
Additional Causes of Excess Oxalates
Oxalates aren’t just a problem for those with gluten sensitivity. Other chronic conditions cause gut inflammation, malabsorption, bacterial imbalances, and so on. Plus, below are two additional reasons why you might experience oxalate-related issues.
Seasonality and Healthy Food Trends
Oxalate poisoning has been documented since the
1850s. It was called oxalic acid diathesis. And it would occur mainly in Spring and Summer months when fresh greens were available.
But until modern times, these high oxalate foods were only consumed when they were in season, which helped prevent oxalates from building up and causing problems in most people.
Today, on the other hand, we consume high oxalate foods all year long. For example, spinach is one of the richest sources of oxalates. Historically, it was only available in the Spring. But today, it’s available year-round. And it’s probably the most commonly used “green” added to smoothies consumed by many on a daily basis.
In addition, almonds are rich in oxalates. And almonds, almond butter, and almond milk are also frequently used in green smoothies.
For perspective, a normal daily intake of oxalates is around
100 – 200 mg. And one green smoothie with spinach can contain up to 1000 mg of oxalates.
Other popular “superfoods,” such as turmeric, chia seeds, cinnamon, cacao, and green tea are also high in oxalates. So for some, these “healthy” trends might not be so healthy after all.
Vitamin C & Oxalates
Ascorbic acid, a form of vitamin C, can be broken down and
converted into oxalates. However, it’s almost impossible to get too much vitamin C from food. In fact,
studies have found no association between dietary vitamin C and the risk of developing kidney stones.
In terms of vitamin C supplementation, study results are mixed. There is some
evidence that high daily doses of vitamin C are associated with an increased risk of kidney stones in men, but
not in women.
Nevertheless, if oxalates are a problem for you, it’s something to consider. You may need to test your vitamin C levels and work with your doctor to adjust your dose.
Are Oxalates to Blame?
You may be wondering whether or not oxalates are to blame for your unresolved health issues or symptoms. If so, I recommend talking to your doctor about the following:
- Testing for high levels of oxalates in your urine – However, a normal result doesn’t mean your body isn’t burdened with oxalates. Your kidneys may not be filtering them properly. And as I mentioned previously, oxalates can build up throughout the body. So if your test results are normal or even low, don’t rule oxalates out.
- Genetic testing for gluten sensitivity, as it has been linked to increased oxalate toxicity issues.
- Testing for gut bacteria composition, which may identify a lack of oxalate degrading bacteria
- Testing for yeast and fungal infections because they may be sources of oxalate production. For example, science has found that the fungus Aspergillus is capable of producing oxalic acid. If infections are discovered, antifungal treatments may be needed.
- Testing for nutrient deficiencies and excesses – Vitamin B6 is important to assess because it can help prevent the formation of oxalates in your body as well as help degrade them. When oxalates are high in your blood, they bind to calcium and magnesium and can cause deficiencies as I mentioned previously. Zinc and iron are worth testing since oxalates can bind to them. Testing for excess vitamin C (ascorbic acid) may also be valuable. Because it can be converted to oxalates, especially when copper is high.
- Supplementation – Calcium citrate taken with meals may help bind oxalates in your gut and prevent them from being absorbed. Vitamin B6, calcium, and magnesium supplements may be necessary to overcome deficiencies, especially during the healing process.
In
this study, patients were given both vitamin B6 (pyridoxine-HCl) and magnesium oxide supplements for 4 months. The researchers reported a gradual, yet significant decrease in oxalate excretion over time.
You can also add foods rich in these nutrients to your diet. For example, fish is an excellent source of both vitamin B6 and calcium.
When it comes to magnesium, many foods that contain high concentrations are also high in oxalates. However, some safe options include broccoli, cauliflower, cabbage, flaxseeds, pumpkin seeds, sunflower seeds, winter squash, and romaine lettuce.
EDTA is a chemical that binds to minerals and can help eliminate them from your body. And
research shows it may be helpful in dissolving calcium oxalate crystals (a.k.a. kidney stones) in the kidneys.
N-Acetyl glucosamine has been used to help
reduce pain associated with oxalate toxicity.
Animal studies have shown that
chondroitin sulfate may help prevent the formation of oxalate calcium crystals in the kidneys. Other animal studies have also had success with
selenium and vitamin E supplementation.
Probiotics may help increase the concentration of oxalate degrading bacteria in the gut.
Omega-3 fats have been shown to
reduce the amount of oxalate excreted in urine and
reduce the risk of kidney stones. The best sources of omega-3 fats are fatty fish (e.g., salmon and sardines) as well as
high-quality fish oil supplements.
Since oxalate toxicity is an acidic condition, alkalinizing substances may also be useful. These include sodium bicarbonate (baking soda), lemon juice, and unrefined salt (e.g., pink Himalayan salt).
A low oxalate diet
Since oxalate urine testing isn’t always reflective of what’s going on inside your body, one of the best ways to determine whether oxalates are a problem is by significantly reducing your intake. Then, see if your symptoms subside over time.
The goal is to get down to approximately 40 – 60 mg of oxalates per day. However, it’s important to reduce your intake slowly. Because a drastic drop can be dangerous, which is why I always recommend working with a professional.
On a low oxalate diet, it’s also important to drink plenty of water to help eliminate oxalates through your urine.
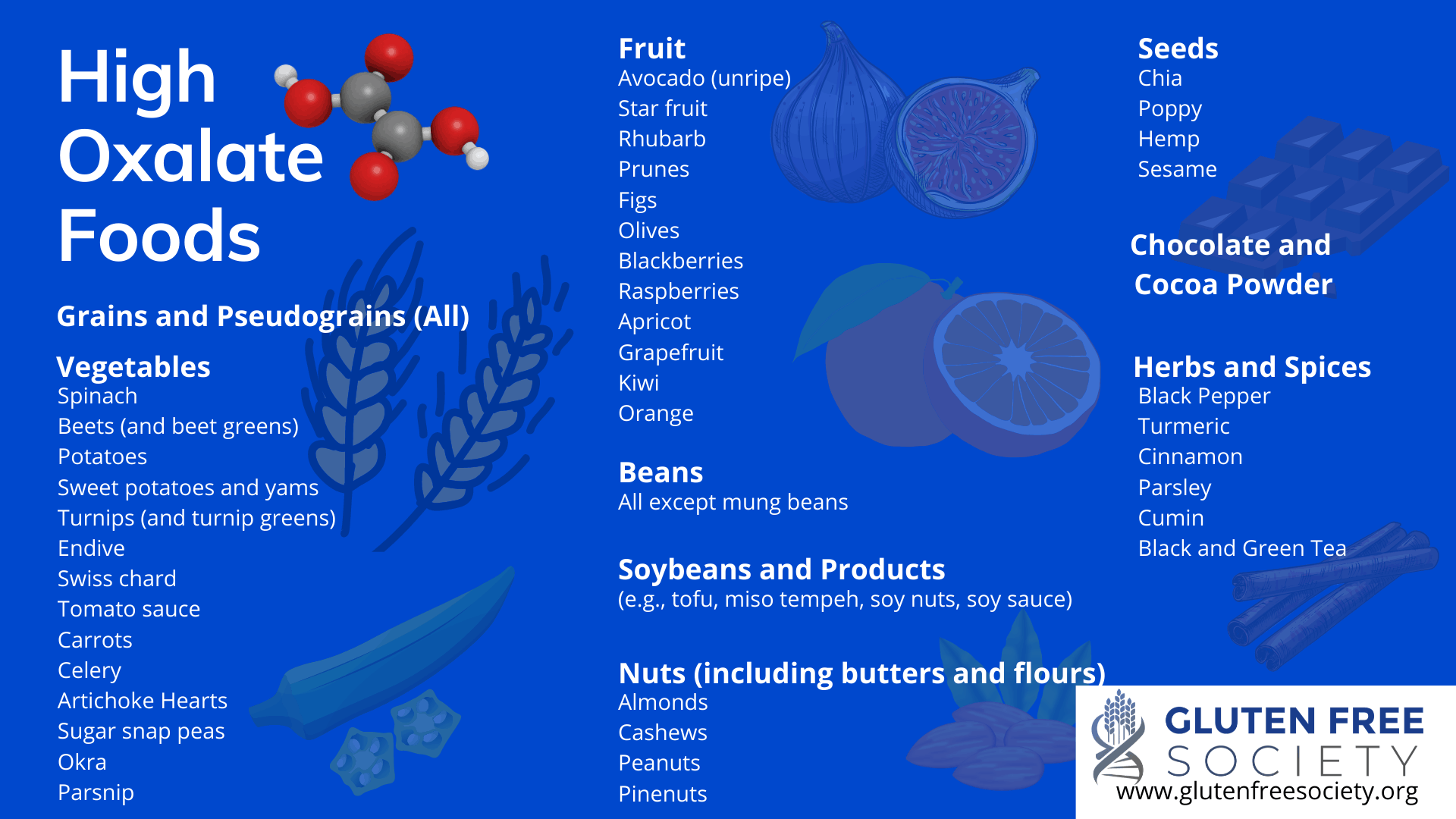
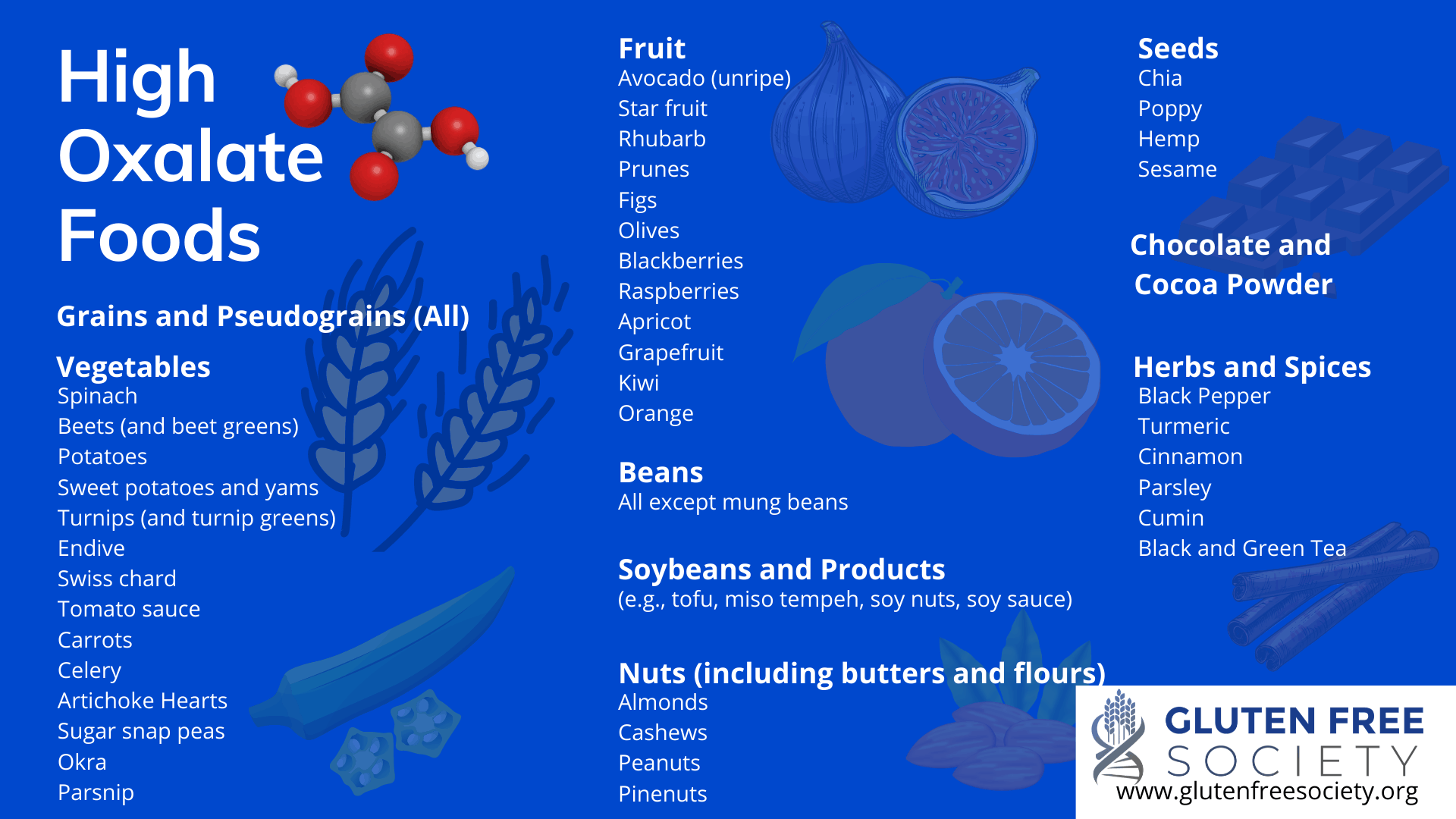
High Oxalate Foods
If you decide to try a low oxalate diet, you’ll want to start by slowly eliminating the following foods:
Grains & Pseudograins (all)
Vegetables
- Spinach
- Beets (and beet greens)
- Potatoes
- Sweet potatoes and yams
- Turnips (and turnip greens)
- Endive
- Swiss chard
- Tomato sauce
- Carrots
- Celery
- Artichoke Hearts
- Sugar snap peas
- Okra
- Parsnip
Fruit
- Avocado (unripe)
- Star fruit
- Rhubarb
- Prunes
- Figs
- Olives
- Blackberries
- Raspberries
- Apricot
- Grapefruit
- Kiwi
- Orange
Beans (all except mung beans)
Soybeans and Products (e.g., tofu, miso, tempeh, soy nuts, soy sauce)
Nuts (including butters and flours)
- Almonds
- Cashews
- Peanuts
- Pinenuts
Seeds (including butters)
Chocolate (and Cocoa Powder)
Herbs and Spices
- Black pepper
- Turmeric
- Cinnamon
- Parsley
- Cumin
- Black and green tea
Grain-free Flours
If you’re following a grain-free diet, it’s important to note that some grain-free flours are also high in oxalates. These include:
- Nut flours (e.g., almond and cashew)
- Arrowroot powder
- Green banana flour
- Potato flour
- Tapioca flour
Thus, coconut flour and potato starch (not flour) are the best low oxalate options.
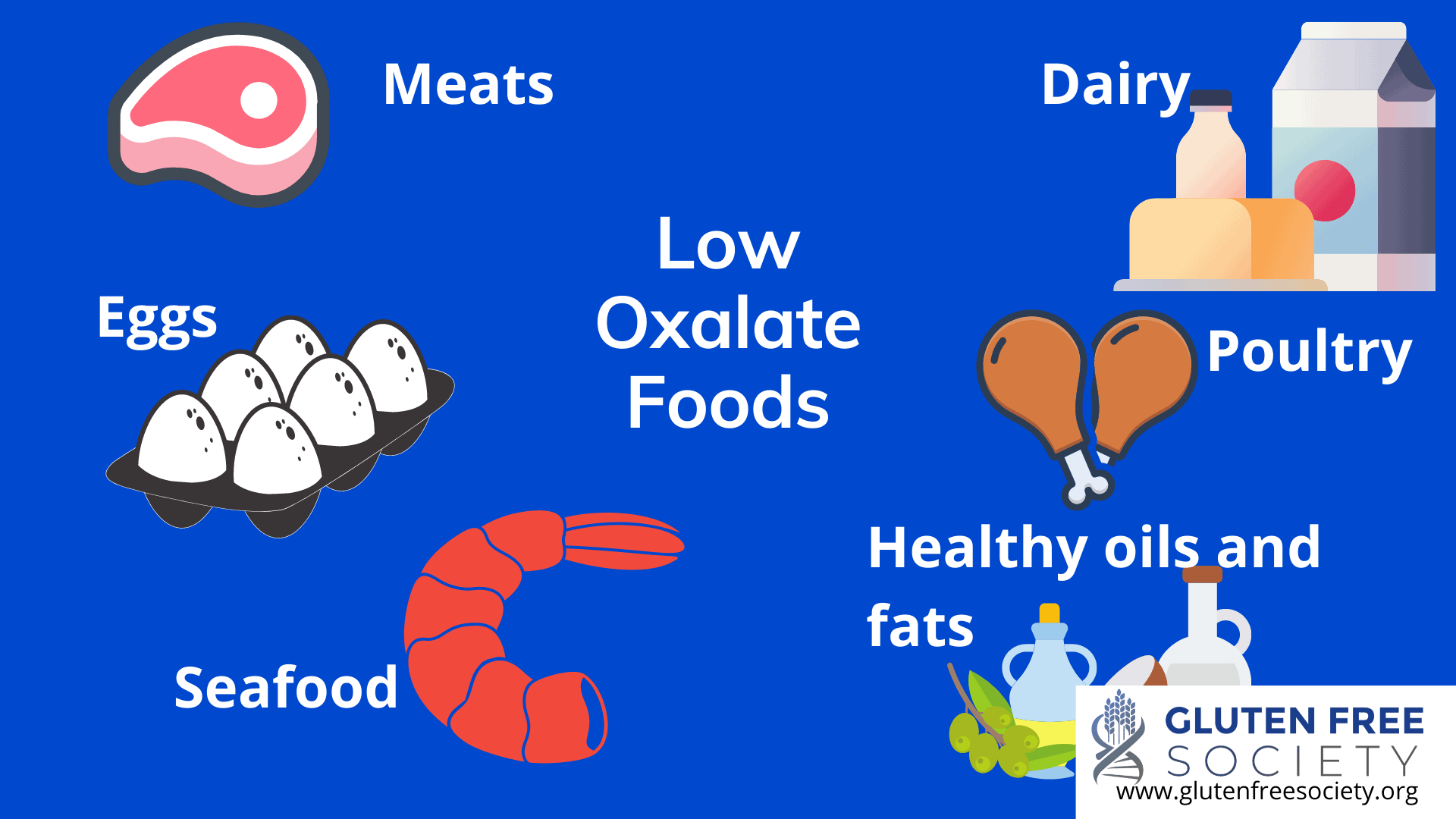
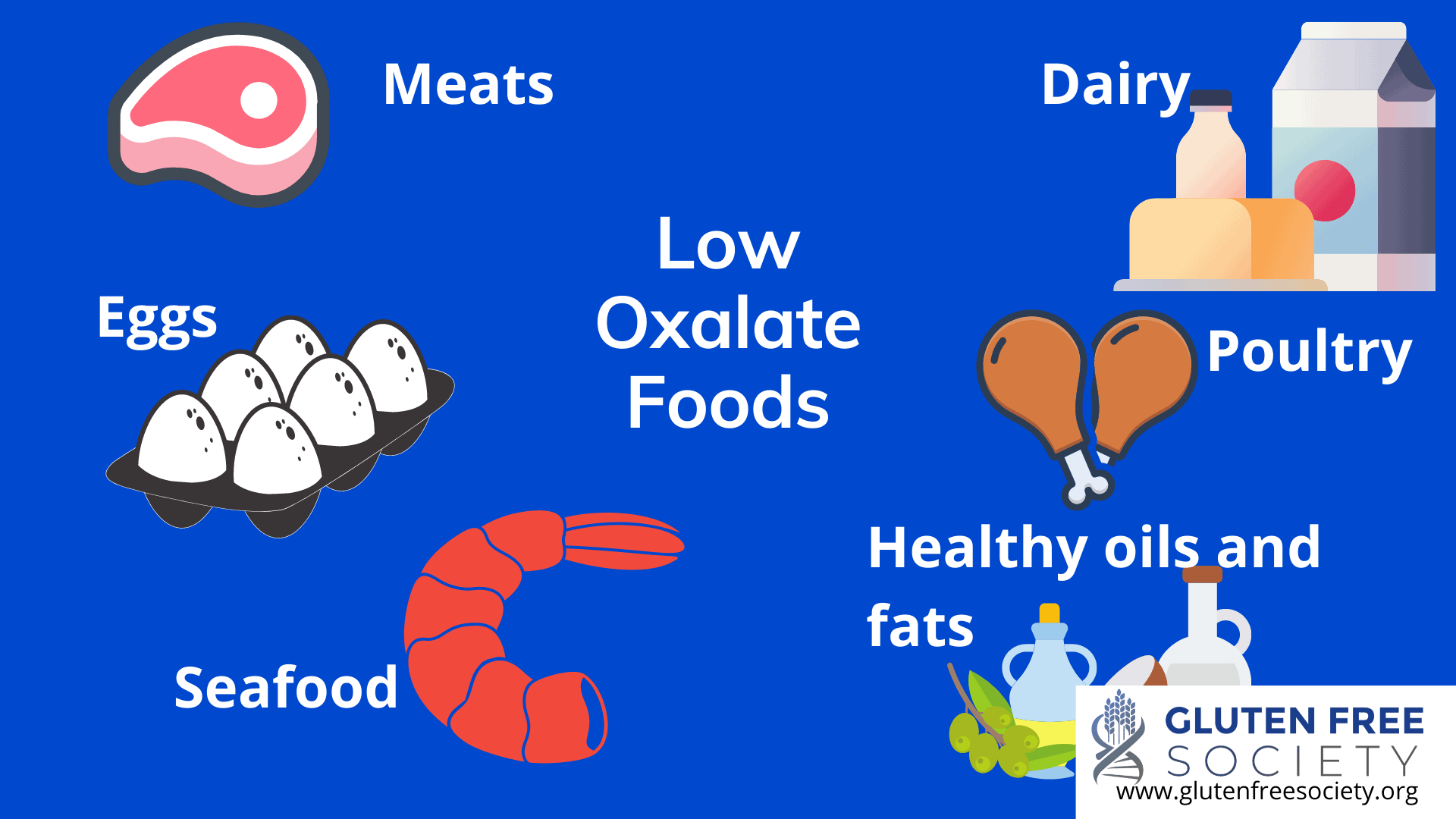
Low Oxalate Foods
The list above may seem long, but there are plenty of low oxalate foods to choose from.
Meats, dairy, poultry, eggs, and seafood are all low in oxalates.
Healthy oils and fats, such as olive, coconut, avocado, and grass-fed butter and ghee are great. However, don’t overdo it! Especially if your gut is compromised. Because poorly absorbed fats in your intestines may cause more oxalates to be absorbed into your bloodstream.
Other good food choices to reduce oxalate burden include:
Vegetables
- Asparagus (boiled to reduce oxalate content)
- Broccoli
- Cauliflower
- Romaine and other types of lettuce
- Arugula
- Cucumbers
- Winter and summer squash
- Red bell peppers
- Lactinato kale
- Squash
- Mushrooms
- Cabbage
- Onions
- Green peas (boiled)
Fruit
- Apples
- Avocado (ripe)
- Grapes
- Cherries
- Plums
- Peaches
- Melon
- Mango
- Papaya
- Blueberries
- Bananas
- Coconut
Seeds
- Pumpkin
- Sunflower
- Watermelon
- Flax
Herbs and Spices
- White pepper
- Basil
- Cilantro
- Honey
- Mustard
- Cardamom
- Dill
- Fresh garlic
- Peppermint
- Cayenne
- Sage
- Thyme

To Sum it Up
Because oxalates are natural and found in healthy foods, their potential for harm is often overlooked. However, there’s
evidence that those with unresolved symptoms and conditions may benefit from reducing their oxalate intake. This includes those with celiac disease and gluten sensitivity when a gluten-free diet isn’t doing the trick.
Some people may also find that when they switch to a healthy gluten-free diet, their symptoms get worse. And oxalates may be to blame. Especially if the diet still includes “gluten-free” grains and green smoothies become a daily staple.
Thus, a grain-free, low oxalate diet may be necessary in some cases to heal your gut and reduce your oxalate burden. So if that’s determined to be true for you, I recommend working with a professional to ensure your plan is safe and effective.
Prefer learning with video? Check out my
video master class on oxalates and the gluten free diet.
Did you benefit by reducing oxalates from your diet? Comment below.
 High oxalates on a gluten free diet might be the mistake that holds your progress back. Do you ever feel like you’re doing everything “right,” but you’re still not feeling your best? Maybe you’ve given up grains, but your symptoms still persist? Or maybe you’ve started experiencing new symptoms?
If your answer is “yes,” then I suggest learning more about oxalates. Because for some, a gluten-free or grain-free diet isn’t enough. Prefer watching a video to learn? Watch Oxalates and Gluten here.
High oxalates on a gluten free diet might be the mistake that holds your progress back. Do you ever feel like you’re doing everything “right,” but you’re still not feeling your best? Maybe you’ve given up grains, but your symptoms still persist? Or maybe you’ve started experiencing new symptoms?
If your answer is “yes,” then I suggest learning more about oxalates. Because for some, a gluten-free or grain-free diet isn’t enough. Prefer watching a video to learn? Watch Oxalates and Gluten here.
 Other good food choices to reduce oxalate burden include:
Other good food choices to reduce oxalate burden include:


38 Responses
Super good info! I have been gluten free, grain free, legume & nut free & dairy free for almost 3 years and just never really see change in how I feel as I try to manage my connective tissue autoimmune disease. But a lot of the foods I eat very regularly are high in oxalates I am seeing. Plus I do a higher dose of oral Vitamin C. Taking the oxalate foods out of my diet slowly as suggested has made a difference in 5 days. Added calcium & krill for omega 3.
Love that you are noticing improvements Pamela! Thanks for sharing your experience!
All the best,
Dr. O
Be careful w vit c as it can convert to oxalates.
Want to try this plan but need an oxalate counter to monitor my intake 40-60 a day.I just had a physical and I have oxalate crystals in my urine but my doctor hasn’t said anything about it!i have had some skin issues lately so I’m ready to give this a try thanks so much 😊
I am tying to eat a grain free diet, but its hard to find grain free foods that also include almonds or almond flour which I am allergic to. Any suggestion?
Butternut flat bread is great and eggs, oil, salt, squash and coconut flour
Casava and Coconut flour are my go to especially for baking. 🙂
I stopped eating legumes a year ago and thought I could introduce them back in. I am sorely mistaken! I have to cut them out again.
My Name is Vanissa Parker, I am so confused on what to eat. I feel terrible everyday. The things I thought were good for me if find out on the blog is bad for me. I try vegan and that’s not working for me either. It there a place or a person I can talk to.
Vanissa, are you going to try eating low oxalate? I have already done AIP diet and that is a big step forward toward low oxalate and it helped me A LOT!! Now I am going even further and taking out more oxalates. There are other doctors out there like Saladino who are showing that all animal foods (carnivore) is safe and healthy and I might even try that at some point, depending on my results.
https://www.semanticscholar.org/paper/Lost-Seasonality-and-Overconsumption-of-Plants%3A-Norton/587548f7a3e96e9173be688689d5e0b013791a07
https://autoimmunewellness.com/recipes/ but also see Jaime at Gutsy by Nature – and she also does consultations with patients
https://www.facebook.com/groups/donteatthatblog/ – this is people who are trying to do Carnivore, so look over the posts there. I’m in that group right now.
If you also have high histamine (“allergy” type symptoms), I have healed myself from that and you can find me on instagram at @histaminehacker Please look over the posts and then direct message me. I am not selling anything or trying to build a business–it’s just me.
I should have said, “Eating ONLY animal foods (carnivore)” not “eating all animal foods” because certainly not all animal foods are safe, but if you do eat only animal foods, then you have drastically reduced your oxalate intake.
Unfortunately, going carnivore for people with coronary artery disease is a no- no. I was on a keto diet for migraines for a couple of years and had to stop due to a severely blocked carotid artery. The fat saturation in many of the keto foods caused the dilemma, along with a DNA loaded with poor markers for high Lipoprotein A markers, which indicate the strong possibility of coronary artery disease. Good luck with your search. I wish you well.
Eating animal fat and meat does NOT cause heart disease or inflammation of the arterial wall, indicated by high lipoprotein A markers. Mostly animal food is the ancestral diet of humans. It’s what our DNA needs and is what made us human and grew our large brain as we evolved from apes to hunter gatherers . Inflammation causes cholesterol, which is made in the liver, to deposit in arteries trying to mend damaged arterial lining. The Hunza tribe don’t have heart disease and their favorite food is meat and organs. Another healthy African tribe eat only meat, blood and milk. Read Dr Saladino’s book. Look elsewhere for the inflammation, including poisons like seed and soy bean oils, plant toxins, glyphosate etc.
Hi Rachel , I’ve just looked on Instagram and can’t find you under @histaminehacker.
You can look up Sally Norton and Elliot Overton. Lowoxalate.info has a pretty robust list of foods. I also made a low oxalate list compiled from Jasmines healing histamine low to medium oxalate list. I can send it if you want.
Low oxalate.info is apparently quite good based on their measurements.
Go real slow in reducing. 4 weeks. 25% reduction a week in diet. You don’t want to get dumping all at once because the body sees an opportunity to get rid of the oxalate when you suddenly stop. It IS prison, crystal like razer structures that damage cells and the likes. So it is paramount to go slow. Shouldn’t take too long, unless you drink spinach smoothies every day, with sweet potatoes every meal, chocolate for lunch and broccoli steamed for dinner, every day 😁🤣. Yeah, that was me a few years back.
If you get a lot of symptoms, add in some more food next meal to stop oxalate dumping. You can always do 100% day one, 75% next day. Then each week decrease it to 75% / 50% etc.
If it’s too much get potassium, calcium or magnesium citrate. You’ll likely be deficient in one or all. Gradually increase amount. Use lemon juice in water gradually increase as well to start flushing out the oxalates. Epsom salt baths for feet should help too.
Elliot overton has a few podcasts and the info is pretty solid. He writes a lot of papers.
Another thing, stinging nettle tea has been linked to stop the binding of oxalates while digesting. Causing it to pass through the body. I drink that with every meal. When i stopped i got really sick because my diet was very high oxalate. I finally figured it out by going on a research bender and reflect on my past symptoms/ health issues. On a reduction diet as we speak and i am in pain all over. My teeth feel like they are going to explode. My gums must have placed oxalate in place of calcium. Still, feel a little better for every day prior to dumping. It usually happens cyclically. For me it’s daily, others may have it weekly or monthly.
Let me know if I can be of any help. It’s not as difficult to try it out to see if it is the actual cause or not. Just gotta be informed properly before trying it.
I forgot to add that the supplements bind the oxalate in blood to stop it from cycling the body and get it flushed as quick as possible. Sally norton’s amount is quite high since most of it gets bound by the oxalates. Best to go really slow and get tested by doc to make sure you don’t overdo it.
Hi Vanissa,
I used to be plant based for 14 years, i will be happy to assist you.
You can contact me at: balanceisperfection.com
I have too much to say about this article LOL so I will just be brief. THANK YOU!! I was already helped greatly by the AIP diet (no grains, seeds, nuts are part of that) and now I am going to try to eat fewer oxalates and even change some of my supplements. Thanks for getting my attention on this. This truly has already changed my life.
About a year ago I started to suffer, for the first time in my 84 years, from excruciating itching, mostly in my face, neck and forearms. After four dermatologists and a skin biopsy , I am still nowhere: each of them put me on a round of oral and topical steroids which relieve the extreme discomfort within days, until it returns full force a few months later. My diet consists mostly of vegetables and lean meat. Has anyone had a similar problem, and has reason to believe that this may be related to an excessive oxalate intake?
I would have recommended that Spinach be totally eliminated, not slowly reduced. A serving of Spinach contains over 700mg of oxalates, and when you consider that a medical textbook I read on PubMed states that a man can have 45 mg and woman only 34 mg of oxalates daily safely, and that higher amounts will without fail cause kidney damage, then Spinach is a toxic nightmare.
I went on a supposedly “healthy” diet and had Spinach twice a day. Well, before too long I was in the ER with back pain over the kidneys and dribbling of urine. A urine test showed sky high oxalates, which sent me on a search to understand oxalates.
Lo and behold, I was killing my kidneys with Spinach. So, now I tell people to put that package of Spinach down and walk carefully away, it is pure Kidney Disease being pushed as a Superfood. Superfood my butt, it is dangerous to your health and should have a Skull & Crossbones printed prominently on the front of each package.
I have watched my oxalates before and it has helped a lot. I’m going to go back on the low oxalate diet because I’m having oxalate crystals in my urine and have had a few big kidney stones in recent years. Do you know if high oxalates have any effect on neuropathy or neuroma? As I’m under treatment for both right now.
Kathryn,
High oxalates can contribute to nerve symptoms including neuropathy. You can read a case study on this in the medical literature right here.
All the best,
Dr. O
Dr O, Thank you so much for this very helpful article. I’ve been gluten free for 10 years. I went grain free this summer and now through this article stopped eating all high oxalate foods. It has helped with my neuroma and neuropathy. Also has helped my mood. Thank you for all your help. I will see a urologist in 2 weeks to see what my oxalate crystals look like in my urine and to get a CT scan in case I have more kidney stones. Looks like I will have to continue on this low oxalate diet for life.
Again thank you. I’m so appreciative of your books and articles. – Kathryn
Not sure whether to laugh or cry…this was flagged as a ‘small diet tweak’…
It essentially rules out nearly everything I eat in my coeliac diet! And I know, after a biome test that I do not have any oxalobacter bacteria! And I do have fat malabsorption. So far I do not suffer much in the way of any symptoms but have always had the feeling that there is a truck behind me …waiting to run over me when I least expect it!
After several requests of my MD…she has finally tested to find I am deficient in fat soluable vitamins….and other stuff! 😣 she always said…..’but you are so healthy!’.
My advice…pun intended….go with your gut instinct! I knew there was a problem.
I am so thankful to see this article here! I have visited your office along with many other Functional Med docs and gynecologists and no one could help or tell me why everything I was doing that was “healthy” was not helping, after 5 years! Praise God I somehow stumbled upon oxalates. I now eat a totally animal based diet, no dairy though and have seen dramatic results. Now if I can just reduce my stress level I think I’ll be doing a-ok! Thanks for your research and posting this!
Thank you for the information you’ve provided on oxalates. I develop kidney and bladder stones fairly often and each time I ask the gastroenterologist what to avoid and I never get a straight answer. I’m going to follow the low oxalate food chart and see if these stones reduce. Again, I really appreciate you!
Let me know how it goes!
Actually it’s my urologist not gastroenterologist that follows my kidney stones!
Is alcohol able to be consumed in a low oxalate diet? If so, which is the best to drink and which alcohol beverages should be avoided?
Is alcohol able to be consumed in a low oxalate diet? If so, which is the best to drink and which alcohol beverages should be avoided?
Is alcohol able to be consumed in a low oxalate diet? If so, which is the best to drink and which alcohol beverages should be avoided?
How do you get a microbiome test that checks for any oxalobacter bacteria? I cannot find any company via Google that does this test. I am based in New Zealand so it will have to be a company that will accept international samples.
I’m late to the game. Celiac diagnosed 22 yrs ago. Can you speak about Tapioca starch. There is so much conflicting info out there (old data that does not get updated but still lingers on the web. What’s true now?) If potato starch (not flour) is low oxalate, why is tapioca starch high? The Wizards of Ox have told me eating dairy with medium to high oxalate foods will not work to bind the oxalate, but now youre saying taking Calcium Citrate does work to bind ox?