new to the gluten free journey?
new to the gluten free journey?
Contents
Toggle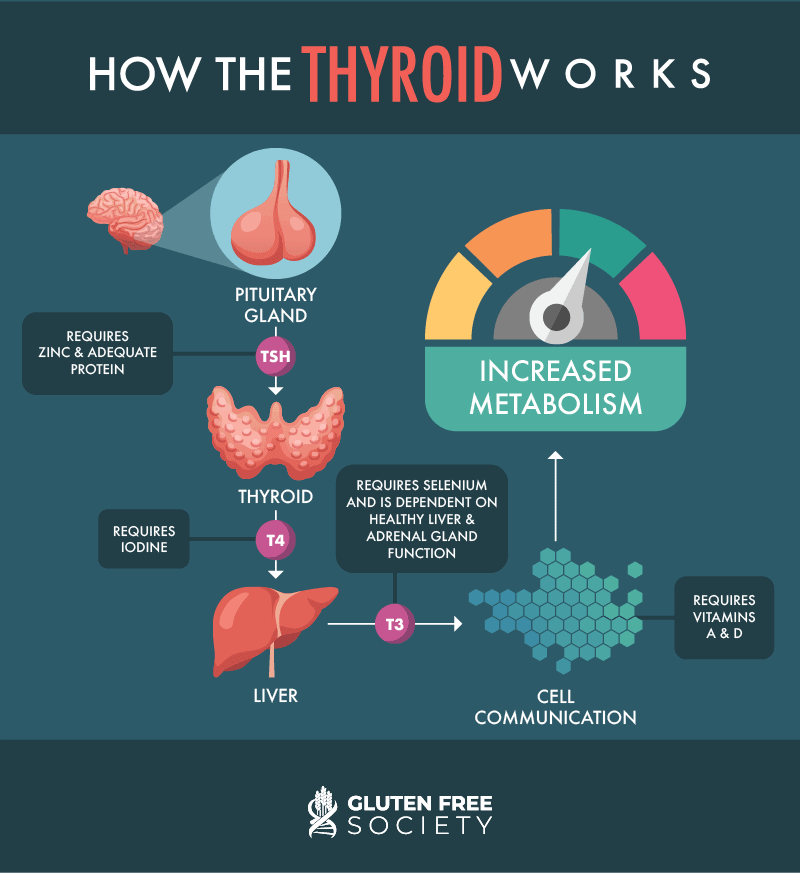
Stay up-to-date with the latest articles, tips, recipes and more.

*These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure or prevent any disease.
If you are pregnant, nursing, taking medication, or have a medical condition, consult your physician before using this product.
The entire contents of this website are based upon the opinions of Peter Osborne, unless otherwise noted. Individual articles are based upon the opinions of the respective author, who retains copyright as marked. The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Peter Osborne and his community. Peter Osborne encourages you to make your own health care decisions based upon your research and in partnership with a qualified health care professional.
16 Responses
You said T3 communicates with DNA. What is going to happen to people getting vaxxed and becoming transhuman with DNA it can’t communicate with? Thanks for the information. Ruby Edmondson
Please don’t worry! – the vaccines don’t really contain trans-human DNA; that’d be waaaay too expensive!
(& I note that Dr. O. hasn’t replied to this one.)
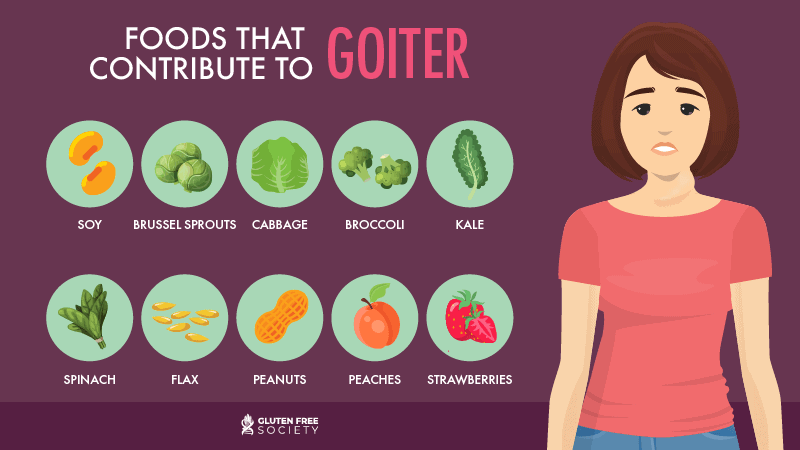
What’s the mechanism between high insoluable fiber causing goiters? Recently diagnosed w ith nodules, would love to shrink these b4 someone gets the bright idea to do surgery on an enlarged thyroid gland, but doesn’t look like oxalates or lectins, then what? gut bacteria being overfed fibers? too much buyterate?, (gluten-free and nearly grain-free for 10 years). Thanks.
You might find this article helpful – https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC4740614/
All the best,
Dr. O
Thanks Dr. O! Appreciate your reply – appears more than a few factors may be involved.
great information..thanks a lot.
Great, informational article! Thank you so much Dr. Osborne! I am gluten-free, I have Hashimoto’s and IBS -D Researching if I have hydrogen SIBO. My understanding is lactobacillus contributes to diarrhea?
Most lactobabilli contribute to healthy guts, so not to diarrhoea.
Oops, please pardon hurried typo! – I meant lactobacilli.
Hi, Thanks for the information. I am, however, very confused. I don’t see how what causes/exacerbates Hashimoto’s is the same as Grave’s. This doesn’t make sense to me. E.g. I have met someone who effectively managed her HYPOthyroidism by diet alone staying off broccoli etc but when reintroducing these went back to being hypo. I don’t understand, do they not then help a HYPERthyroid condition? Similarly should I avoid food that has higher iodine levels in it like Seafood? If I have Iodine supplements surely that will aggravate Grave’s? I have had Grave’s on and off for a few years now and I am really trying to find an alternative to medication and radio iodine or surgery. The consultant endocrinologist is pushing me towards radio iodine but I have an absolute horror of the idea of knocking out my thyroid for good and consequently being on medication for the rest of my life. Any clarification would be very welcome.
Any information on Thyroid cancer and thyroid nodules would be appreciated
Appreciate reading your book, No Grain, No Pain, very much. You mentioned vitamin B1, B2, B5, and B8 which I’ve never heard of. Nor can I find my multivitamin supplement Centrum Silver include them. Where can I find those four B vitamins? Are they in B Complex supplement? Thanks.
Here you go Valerie – https://env-gfsociety-staging.kinsta.cloud/shop/supplements/general-health/b-complete/
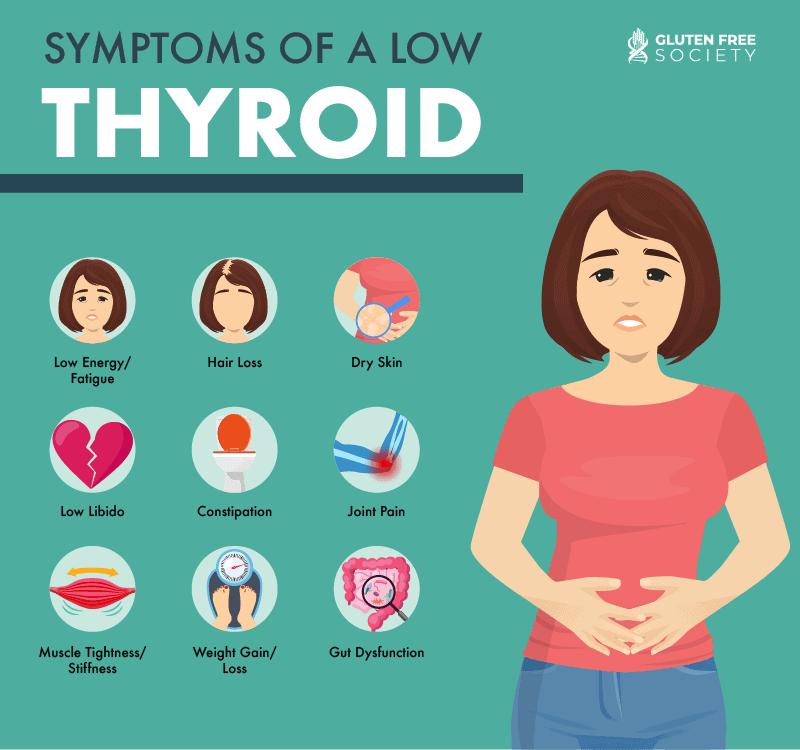
What are the symptoms that can be detected early for thyroid sufferers who may not be aware that they have the disease?
thinning hair or eye brows, sensitivity to cold, dry skin, to name a few. Believe doc listed some of these as well maybe in his ebook or elsewhere, but symptoms can easily be searched online.
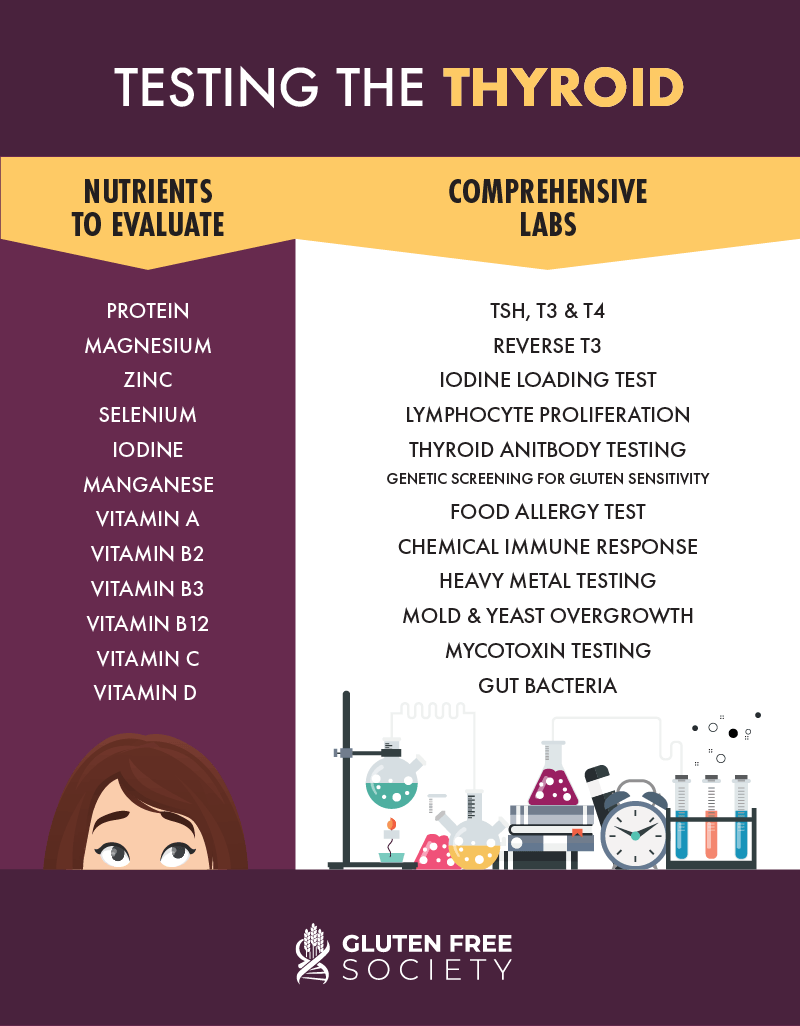
I was diagnosed with hoshimoto thyroid years ago and have been taking 350m of levetheroxine for years because Dr’s say my levels are dangerously high. How can I get this under control. I have been on a carnivore diet for 1 month now, so I have cut out a lot listed in your article. What test should I request from my dr.