new to the gluten free journey?
new to the gluten free journey?

Contents
Toggle
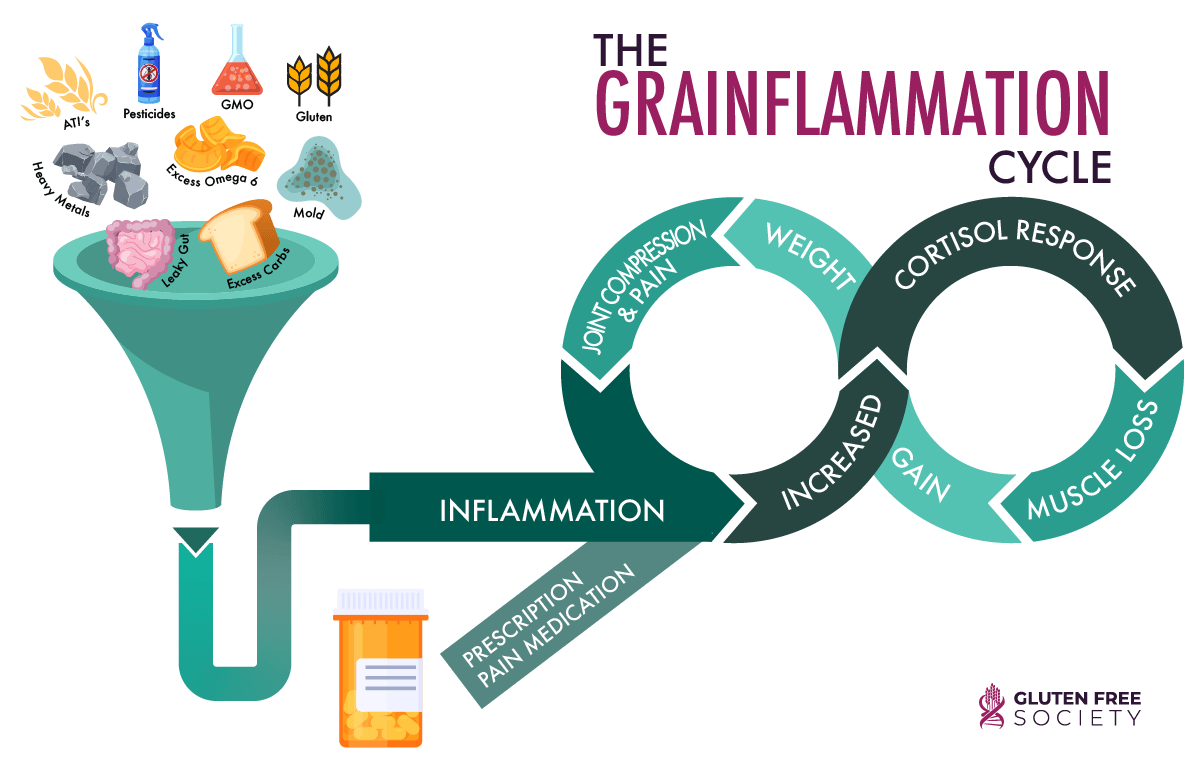 Furthermore, many undiagnosed celiac disease or gluten sensitive individuals learn to rely on acid blocking medication to reduce or manage their confusing and disruptive digestive symptoms. These medications reduce stomach acid and further impair protein digestion.
Furthermore, many undiagnosed celiac disease or gluten sensitive individuals learn to rely on acid blocking medication to reduce or manage their confusing and disruptive digestive symptoms. These medications reduce stomach acid and further impair protein digestion.
Stay up-to-date with the latest articles, tips, recipes and more.

*These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure or prevent any disease.
If you are pregnant, nursing, taking medication, or have a medical condition, consult your physician before using this product.
The entire contents of this website are based upon the opinions of Peter Osborne, unless otherwise noted. Individual articles are based upon the opinions of the respective author, who retains copyright as marked. The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Peter Osborne and his community. Peter Osborne encourages you to make your own health care decisions based upon your research and in partnership with a qualified health care professional.
14 Responses
My phone died during ur video on protein deficiency. I am having severe problems with corn. I noticed that threonine is a hidden source of corn. Is threonine in collagen peptides made from corn?
Depends on the source of collagen peptides. Corn is not typically used if collagen is derived from animal sources.
Im curious, if a general problem with protein digestion and absorbtion in yhe intestines is related to long term undiagnosed celiac disease, why recommend increased protein intake rather than enzymes? Also, are there some proteins that are more challenging to digest? Where can i find your sources for this article? I would like to read more about the topic. Thanks!
Hi Alyx,
Gluten can damage the small intestine, liver, and pancreas. This damage can cause maldigestion/absorption issues. The most important solution is to remove gluten from the diet. Digestive enzymes can be taken for support, but real healing happens with the diet change. All of the blue text in the article are links to research studies and sources.
Have a great day!
Dr. O
I know I am Coeliac. Handed down generations. I do my best to eat as much protein as possible..
Protein gives me really bad constipation. Is there an easier form of Protein that I can take?
Chris you might try 2 things:
1. Ultra Acid – This supplement will support your ability to properly digest protein.
2. Warrior protein – this is an organic plant based protein that is easy to digest.
This is fascinating! I noticed the palms of my hands get red and blotchy from time to time and all I could find was Palmar Erythema (which is what it looked like exactly) and liver cirrhosis. But I don’t have that. Then I found very old scientific papers based in the 1940s or earlier that stated they noticed this phenomenon when n some remote countries or villages where protein wasn’t eaten enough and once they increased their protein intake it resolved. So low and behold I increased my animal protein intake, because it seems I don’t absorb plant protein well at all, which is what landed me to have these symptoms in the first place, and sure enough my symptoms resolved completely upon increasing my animal protein intake. It’s frustrating though because I would like to be more plant based but for some reason, probably the gluten intake most of my life (resulting in damage) has prevented me to do so.
Thank you for this. I have not been able to find many current blogs or content on the relation between celiac/gluten and protein deficiency
Kind of curious as to why many (some do) don’t calculate protein requirements based on lean body mass rather than total weight. LBM is where we need the protein, not adipose tissue. Just sayin’. Any thoughts? Thanks.
Just What I Needed To Read About Protein!!! 3/17/2022 I Received An Ileostomy – Surgery Went Well & I Love My “Jilly”!!! I’ve Been Gluten,etc., Free Since 1995!!! Before My Surgery, I Had To Build Up To 120 lbs. To Have The Operation – My Diseased Colon Removed Weighed 25 lbs. Not To Say The Least, I Had Major Serious Colon & Rectum Problems – I Came Home At 87 lbs. & Stayed That Way For 8 months!!! My Food Sensitivities Are Off The Charts – I Just Recently Gained 7 lbs. By Adding Quite A Bit Of Almond (SAFE) Cheese – It’s All Almond!! I Don’t Know If I’m Overdoing It Because I Gain A Pound A Week – So Fast!!! I’m 66 yrs. old, 5 Feet, 93 lbs. – Goal Is 95 lbs – I Forgot To Mention That I Only Eat 10 Different Foods- OCD, Depression, Anxiety, MAJOR MIGRAINES, My Recent Thyroid Results (AND I’VE HAD HYPOTHYROIDISM FOR 35 yrs.) Came Back Extremely Lower Than The Low I Already Have. Dr. Doesn’t Feel We Should Increase My Synthroid So I Did It Myself!!! That May Seem Crazy But Because My Hot Flashes Returned 3 mnths. (I WENT THROUGH MENAPAUSE IN MY EARLY 50’S), MIGRAINES ON A RISE AT A RAPID PACE, & OTHER SYMPTOMS HAVE SURFACED!!! I DID A DESPERATE MOVE BUT I FEEL A SHIFT – GOING TO GET KETAMINE TREATMENTS FOR MEDICATION RESISTANT DEPRESSION (ALMOST 40 yrs. – NO DRUG WORKED – Went All Through Trudy Scott’s Amino’s – No Luck!!! I’M USING CBD FOR ANXIETY LATELY – BUT THAT HELPS ANXIETY NOT DEPRESSION – ANY HELP & ADVICE FROM YOU WOULD BE GREATLY APPRECIATED – I Forgot – I Eat Eggs & Chicken – All Ingredients AOK!!! I’VE BEEN FOLLOWING ALL OF YOUR WORK FOR A LONG TIME!!!! PLEASE HELP – SOS!!!!
Hi Gluten Free Society,
My name is Scott. I was diagnosed Celiac in 2008, I was 35 then. I was diagnosed with the blood test and via a sample taken from my intestine which confirmed the diagnosis and indicated an approx 40% loss or score of 2 out of 5 for intestine damage. I also had a liver ultrasound done that indicated my liver was much larger than it shuold be. I don’t consume alcohol. I also had a bone density test that confirmed Osteopenia and I recently had a protien absorbtion test done for the first time which indicated low protien levels which was a surprise since I’m consuming high amounts of protien with my regualr food diet and via supplementation. I’m regularly feeling inflammed with tight joints. So with all that informaiton in mind my quesiton is do you know of any highly respected and informed celiac nutritionists that you’d be able to recommend to help me create a diet plan. I think the time has come that I stop trying to figure things out on my own. Thanks in advance.
Scott,
Sorry to hear that you are going through this. You might consider reaching out to Dr. Osborne’s practice – 281-240-2229
i am vegan but totally protein deficient, my nails are brittle and i have all the symptoms.
i would like to buy your protein but i cannot find a link to it.
would you please send it to me ?
thank you for your work and information. Much appreciated.
Dagmar
Thank you for this article.
I have had a lot of problems with gluten and went gf a couple of years ago and feel so much better.
I always get drawn into plant based diets and no matter how many different types of beans, nuts or tofu I eat, I get weak and start craving sweet foods constantly. This leads to insulin resistance and feeling ill, brittle, weak nails with lines, tiredness etc.
I decided to eat a good meal of chicken and straight away the sugar cravings went and over time increased strength and energy came back.
Not sure weather a damaged gut prevents protein absorbtion or I just need a good quality decent amount of protein. somewhere around a gram per pound of bodyweight for my active lifestyle.
Thanks
Andrew.