new to the gluten free journey?
new to the gluten free journey?
Contents
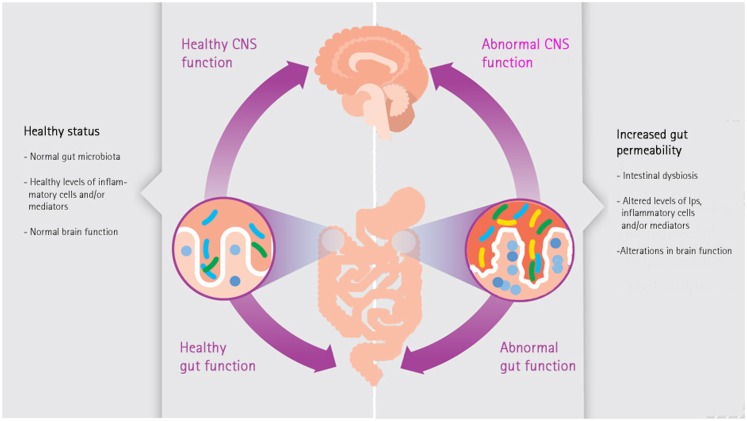
ToggleThe non-celiac gluten sensitivity (NCGS) is a chronic functional gastrointestinal disorder which is very common world wide. The human gut harbors microbiota which has a wide variety of microbial organisms; they are mainly symbiotic and important for well being. However, “dysbiosis” – i.e. an alteration in normal commensal gut microbiome with an increase in pathogenic microbes, impacts homeostasis/health. Dysbiosis in NCGS causes gut inflammation, diarrhea, constipation, visceral hypersensitivity, abdominal pain, dysfunctional metabolic state, and peripheral immune and neuro-immune communication. Thus, immune-mediated gut and extra-gut dysfunctions, due to gluten sensitivity with comorbid diarrhea, may last for decades. A significant proportion of NCGS patients may chronically consume alcohol, non-steroidal anti-inflammatory drugs, and fatty diet, as well as suffer from various comorbid disorders. The above pathophysiological substrate and dysbiosis are underpinned by dysfunctional bidirectional “Gut-Brain Axis” pathway. Pathogenic gut microbiota is known to upregulate gut- and systemic inflammation (due to lipopolysaccharide from pathogenic bacteria and synthesis of pro-inflammatory cytokines); they enhance energy harvest, cause obesity, insulin resistance, and dysfunctional vago-vagal gut-brain axis. Conceivably, the above cascade of pathology may promote various pathophysiological mechanisms, neuroinflammation, and cognitive dysfunction. Hence, dysbiosis, gut inflammation, and chronic dyshomeostasis are of great clinical relevance. It is argued here that we need to be aware of NCGS and its chronic pathophysiological impact. Therapeutic measures including probiotics, vagus nerve stimulation, antioxidants, alpha 7 nicotinic receptor agonists, and corticotropin-releasing factor receptor 1 antagonist may ameliorate neuroinflammation and oxidative stress in NCGS; they may therefore, prevent cognitive dysfunction and vulnerability to Alzheimer’s disease.Other Studies have shown that gluten can alter the normal bacterial flora, and in doing so set the stage for decreased levels of regulatory gut bacteria, and increased levels of bacteria that contribute to inflammation. When you combine leaky gut with altered bacteria, you get an increased presence of bacteria and their by products in the blood. One type of bacterial byproduct is LPS (lipopolysaccharide). Studies have shown that when this happens, the immune system will produce inflammation trying to combat the presence of these translocated bacteria. This increase inflammation has been shown to alter the function of the brain, and a side effect of this is DEMENTIA.[1, 2] The image below illustrates the connection:
Stay up-to-date with the latest articles, tips, recipes and more.

*These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure or prevent any disease.
If you are pregnant, nursing, taking medication, or have a medical condition, consult your physician before using this product.
The entire contents of this website are based upon the opinions of Peter Osborne, unless otherwise noted. Individual articles are based upon the opinions of the respective author, who retains copyright as marked. The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Peter Osborne and his community. Peter Osborne encourages you to make your own health care decisions based upon your research and in partnership with a qualified health care professional.
4 Responses
Thank you!
Great piece Peter. The thing about membrane hyper permeability (leaky gut, brain etc) is that the whole process has been explained in scientific literature already. Careful analysis of mainstream physiology, biochemistry, anatomy, pathology, nutrition, stress research etc reveals how this condition develops and progresses. Hopefully, mainstream medicine will wake up soon. In the meantime, there is plenty of hope for those who need it, and there is support out there…
My brother died on November 23,2016. He had a form of Dementia. He also had a history of bowel blockages and constipation.
After reading this article I now wonder if his digestion problems were the cause of his dementia.
I am interested in learning more about what to do to regulate the good bacteria in my gut. I have had migraines in the past, periods of severe diarrhea and occasional constipation.
What tests do I need to ask my doctor to do to see what kind of bacteria I have and if it is normal? And if I am gluten sensitive?
I don’t want to be the next victim of Dementia or Alzheimers.
Thank you, Donna Gallentine
Great information. What does it mean to be sensitive to a lot of foods? Is there a connection with leaky gut? Thank you in advance for your answer.