new to the gluten free journey?
new to the gluten free journey?
 A recent research report identified an individual with progressive nerve damage findings mimicking the autoimmune neurological condition known as Lou Gehrig’s disease (AKA – ALS or amyotrophic lateral sclerosis). The condition manifests as progressive muscle weakness and loss, involuntary spasms and twitches, and eventually a degeneration of the muscles responsible for aiding in breathing. Many sufferers of ALS die as a result of suffocation once the muscles of respiration become paralyzed.
There are many theories on the causes of ALS. One prominent suspicion is in a defective antioxidant gene called SOD1(superoxide dismutase). This gene is a powerful antioxidant that is activated by the two essential minerals, copper and zinc. Patients with ALS often have this genetic variant that predisposes areas in the brain and spinal cord to free radical damage.
As ALS is an autoimmune condition, the next question becomes – does gluten play a role in the development or contribute to the disease?
A recent research report identified an individual with progressive nerve damage findings mimicking the autoimmune neurological condition known as Lou Gehrig’s disease (AKA – ALS or amyotrophic lateral sclerosis). The condition manifests as progressive muscle weakness and loss, involuntary spasms and twitches, and eventually a degeneration of the muscles responsible for aiding in breathing. Many sufferers of ALS die as a result of suffocation once the muscles of respiration become paralyzed.
There are many theories on the causes of ALS. One prominent suspicion is in a defective antioxidant gene called SOD1(superoxide dismutase). This gene is a powerful antioxidant that is activated by the two essential minerals, copper and zinc. Patients with ALS often have this genetic variant that predisposes areas in the brain and spinal cord to free radical damage.
As ALS is an autoimmune condition, the next question becomes – does gluten play a role in the development or contribute to the disease?
Contents
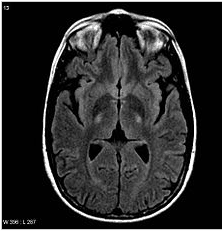
ToggleCD is an autoimmune-mediated disorder of the gastrointestinal tract. Initial symptom presentation is variable and can include neurologic manifestations that may comprise ataxia, neuropathy, dizziness, epilepsy, and cortical calcifications rather than gastrointestinal-hindering diagnosis and management. We present a case of a young man with progressive neurologic symptoms and brain MR imaging findings worrisome for ALS. During the diagnostic work-up, endomysium antibodies were discovered, and CD was confirmed by upper gastrointestinal endoscopy with duodenal biopsies. MR imaging findings suggestive of ALS improved after gluten-free diet institution.Source: AJNR Am J Neuroradiol. 2010 May;31(5):880-1. Epub 2009 Nov 12.
Stay up-to-date with the latest articles, tips, recipes and more.

*These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure or prevent any disease.
If you are pregnant, nursing, taking medication, or have a medical condition, consult your physician before using this product.
The entire contents of this website are based upon the opinions of Peter Osborne, unless otherwise noted. Individual articles are based upon the opinions of the respective author, who retains copyright as marked. The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Peter Osborne and his community. Peter Osborne encourages you to make your own health care decisions based upon your research and in partnership with a qualified health care professional.
4 Responses
My mother died two yrs ago in diagnosed ALS. Eventhough she died at the age of 83, she had CD for a long time undiagnosed from her thirties – forties. Then diagnosed CD. I haven’t eaten bread, pasta or any type of gluten containing food since. And I don’t miss it. Its not worth it. Anyone who have had an ALS diagnosed person close by would understand this.
My dad died of ALS complications in 2011. He had all of the symptoms of gluten intolerance. I have been eating G-F for almost 14 years and obviously will continue to eat this way for my whole life.
Hello,
My husband was diagnosed with ALS 2010 ( by the most arrogant female doctor you would never want to meet),
thankfully I felt, after a set of questions and a bit of a physical exam, not even the greatest neurologist in the world could possibly diagnose ALS that quickly. She told us to get things sorted. Fortunately we have been under the care of a fantastic natural (whole of body) doctor. No ALS, just gluten sensitivity plus hyperthyroidism. Please, please do not take the first diagnosis you get as gospel, no doctor in the world is god. My husband is still here and doing well. Our family is GF, it is poison.
I am a CALS. My husband is PALS. It was hard and I cry daily but not in front of him unless we cry together. He couldn’t find anything to give him happiness or hope. We have been focusing on our faith. He was only losing his voice before we made the decision to try different medications, which significantly enhanced his condition. He received treatment for ALS/MND at uinehealth centre . c om from Canada approximately four months ago; since then, he has stopped using a feeding tube, speech is getting better by the day, sleeps well, works out frequently, and has become very active.