new to the gluten free journey?
new to the gluten free journey?
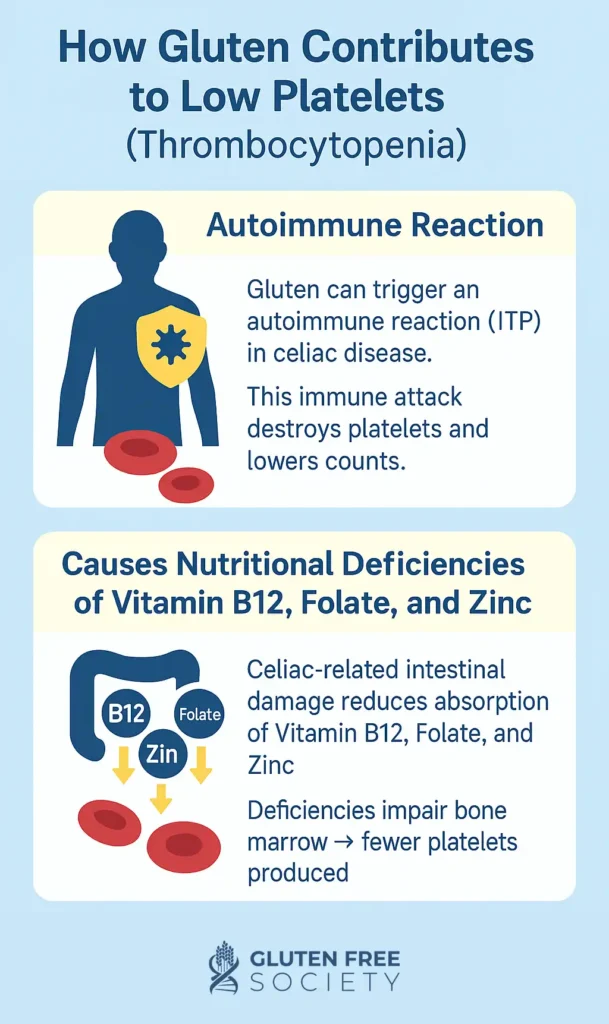
Gluten can lower platelet counts through celiac-induced autoimmunity (ITP) or nutrient malabsorption (especially B12 and folate). Research links celiac disease with low platelets, and many improve on a gluten-free diet. If you have unexplained thrombocytopenia, celiac screening and nutritional testing may be key to recovery.
Contents
ToggleGluten consumption has been identified as a cause of low platelets, most convincingly through celiac disease. Research shows a higher prevalence of immune thrombocytopenia (ITP – AKA low platelets)) in people with celiac disease, and several cases document platelet recovery on a strict gluten-free diet. In addition, folate and B12 deficiencies from small-intestinal injury in celiac disease can reduce platelet production.
Practical takeaway: If you have ITP with no clear cause, screen for celiac disease. If you have celiac plus low platelets, adhere strictly to a gluten free diet and coordinate care with your hematologist.
Celiac disease damages the small-intestinal mucosa, reducing absorption of iron, folate, and vitamin B12. Folate and B12 are required for DNA synthesis in the bone marrow. Deficiency can lead to thrombocytopenia or even pancytopenia. Platelets often recover after repleting the deficient nutrient and removing gluten.
Medical evidence:
People with unexplained low platelets plus any of the following: iron deficiency, anemia, neuropathy, bone pain, chronic diarrhea or constipation, bloating, dermatitis herpetiformis, autoimmune thyroid disease, type 1 diabetes, or family history of celiac disease.
Do you have an experience with improved platelet counts on a gluten free diet? Share your story below.
I commonly see patients with abnormal blood cell counts (red blood cells, white blood cells, and platelets). Many of these patients have never had these abnormalities explained to them by their primary doctors. None the less they suffer with the consequential side effects. Easy bruising, bleeding gums, heavy menstrual cycles, fatigue, brain fog, anxiety, and muscle pains are common symptoms. Often times further investigation reveals that these individuals are gluten sensitive. For these people, going gluten free and supplementing with the right nutrients can lead to complete resolution.
Not directly. The strongest data implicate celiac driven autoimmunity that can present as ITP, and malabsorption related deficiencies that reduce platelet production.
It can in select cases, especially where celiac disease coexists with ITP or with folate or B12 deficiency. Several reports document platelet normalization after starting a gluten-free diet. Individual results vary and require medical supervision.
Yes. False negatives occur if gluten was reduced before testing or if IgA deficiency is present. Discuss biopsy, IgG-based tests, or HLA-DQ genotyping when appropriate.
Folate and vitamin B12 are most often implicated. Correcting these can improve counts. Iron deficiency is common in celiac disease but typically affects red cells; combined deficiencies may occur.
Prevalence estimates vary by study, but ITP occurs more often in patients with celiac disease than in the general population, and screening is reasonable in otherwise unexplained ITP.
Infections, medications, alcohol, liver disease, bone-marrow disorders, and other autoimmune conditions. Work with your clinician to rule these out while evaluating gluten and nutrient status.
Yes, gluten has been linked to the development and increased risk of many forms of autoimmune disease. Medical researchers sometimes refer to these collectively as Non Celiac Gluten Sensitivity and Extra-intestinal manifestations.
Written and medically reviewed by Dr. Peter Osborne. Updated on September 4, 2025
6 Responses
3 years ago DNA test showed celiac. Gluten free for three years and gluten replacements have attacked my body with fibromyalgia and serious arthritis even worse. Working with LEAP certified dietician and having LEAP blood test have turned my life around in three months. Long way to go but finding whole unprocessed foods and eating things I never heard of before. Learning to cook and bake differently. LEAP has been the answer for me!
I find a Paleo diet really addresses the inflammation and with a little gut healing, a person can really heal. Great video!
Can you be gluten sensitive and still be a platelet donor? I have taken the celiac test and it was negative. I keep getting asked to donate platelets. I haven’t for a year now.
I had mishapen white cells 5 years back would this have arousin suspicion of a gluten problem?
I am suffering from thrombocytopenia.
Doctors advised me to go gluten free diet.
Is it really good for me.
I am suffering from low platelet count, low WBC, and hemoglobin. My doctor thinks it’s lymphoma or leukemia. I’m hoping I’m just allergic to gluten.