new to the gluten free journey?
new to the gluten free journey?
 weakened or spooned nails (see the picture on the right)
weakened or spooned nails (see the picture on the right) iron deficiency in several ways. Malabsorption of iron is often a consequence of damage to the small intestine (villous atrophy). Additionally, gluten can damage the acid producing cells of the stomach. Since acid is a necessary component for iron absorption, this commonly leads to anemia even in the absence of villous atrophy identification.
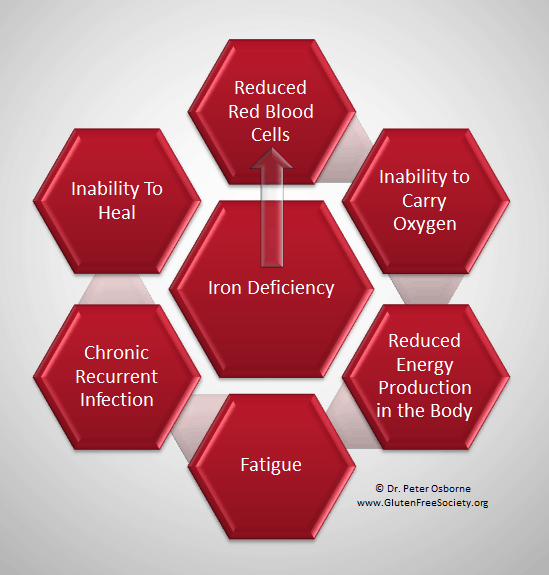
Anemia leads to oxygen deficiency which in turn can reduce the body’s ability to generate energy, which in turn can cause a cyclic state of healing inhibition.
Aside from gluten induced damage, iron deficiency can occur in menstruating women with heavier periods. Iron deficiency can also occur when there is slow steady blood loss. This can occur in a hidden manor (occult blood loss) or it can be more obvious as in the case of hemorrhoids.
iron deficiency in several ways. Malabsorption of iron is often a consequence of damage to the small intestine (villous atrophy). Additionally, gluten can damage the acid producing cells of the stomach. Since acid is a necessary component for iron absorption, this commonly leads to anemia even in the absence of villous atrophy identification.
Anemia leads to oxygen deficiency which in turn can reduce the body’s ability to generate energy, which in turn can cause a cyclic state of healing inhibition.
Aside from gluten induced damage, iron deficiency can occur in menstruating women with heavier periods. Iron deficiency can also occur when there is slow steady blood loss. This can occur in a hidden manor (occult blood loss) or it can be more obvious as in the case of hemorrhoids.
 Lack Of Iron Causes Immune Problems
Lack Of Iron Causes Immune ProblemsStay up-to-date with the latest articles, tips, recipes and more.

*These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure or prevent any disease.
If you are pregnant, nursing, taking medication, or have a medical condition, consult your physician before using this product.
The entire contents of this website are based upon the opinions of Peter Osborne, unless otherwise noted. Individual articles are based upon the opinions of the respective author, who retains copyright as marked. The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Peter Osborne and his community. Peter Osborne encourages you to make your own health care decisions based upon your research and in partnership with a qualified health care professional.
34 Responses
A year ago my new family doctor examined me simply because he didn’t have much on file about me. Then he found out I had a severe iron deficiency. The number was 3 which should be at least 40. It surprised him I felt good. However, he thought the reason for this was that I hadn’t catch up with my severe C-section, now 7 years ago. Starting a treatment with iron tablets and even an iron injection right into the muscle (for which I’m allergic we found out AFTER the injection) didn’t do much. In December I was tested for gluten sensitivity, positive! Started a gluten free diet and my iron was going up! Unfortunately I have been lazy with gluten free last few weeks and my numbers are down to 6.4 from 11.2. I feel very tired which I never did even when my numbers were less then this. Learn the hard way I’m really sensitive to gluten. I’m not sure if I ever can go back to gluten, for now I have to eliminate it from my diet!
Hi its kashif my wife also suffering bcz of her iron level is 3 we are from Pakistan staying in South Africa last night i took her to emergency bcz 2’oclock in the morning she was struggling of shortness of breathing and suddenly she called me and fall down
Please help me out what should i do
What was the issue she had?
Hi Carina,
I have the same problem my iron study show Ferritin is 4 and just rapidly down from point 40 to 4 in a month after stop taking a supplement. He also suspects that I have gluten sensitivity, and this five weeks I will get gluten out of my life as much as possible and have it tested at the end of 5 weeks. I Never heard before gluten intolerance can affect the iron deficiency while researching I came across your post. when do you start to eat gluten-free after how many days did you start to feel better?
thank you for your post,
Gluten sensitivity and celiac are a family trait and 1 in 2 people in my family have it.
I have always been anemic and had no digestive issues until a year ago when I was assaulted and left with 8 concussions and a boat load of extreme stress. Within a week of this I became severely intolerant to gluten. I cant even make a sandwich for my boyfriend without getting sick. I AM THE FIRST IN MY FAMILYS HISTORY TO HAVE GLUTEN INTOLERANCE.
I am celiac. I had extremely low iron when I was first diagnosed. I took iron pills but could not absorb them due to intestinal damage. Finally I had to have iron transfusions.
I am wheat and milk intolerant (extreme for milk), and I have had gastritis, bursitis, costochondritis, anemia, adrenal failure and candida. If iron deficiency is the root of all this, then the key to our lives may be medicinal iron supplementation. However I’ve been taking 500 mg for 2 months and still every day I feel like there is no oxygen in my arms. I’m a 27 year old woman yet my arms feel like those of a 70 year old. No muscles, just sensitive tissue, or at least that’s how it feels, because I’m actually quite strong. Breathing rarely feels satisfying. Should I take more iron? I try to eat a lot of chicken, eggs and rosbif on top of the pills to “cheat” a little and because a various diet is important, but nothing seems to be working. I’m not fatigued anymore but that’s because I take cortisol for my adrenals.
Lenie,
You need to find a good functional medicine doctor to work with. Someone with an intimate knowledge of biochemistry, lab testing, and proper follow up evaluation skills. You might also find the book, No Grain No Pain very helpful.
All the best,
Dr. Osborne
I am hypothyroid. I bruise easily & have had labs done twice now which come back ‘normal’. I take iron supplements which help some.
Now with food diary I’m noticing gas & bloating with gluten/wheat. Recently has first run in with hemorrhoids. I drink plenty of water & run almost daily. Will be cutting out gluten now to see if helpful!
I am hypothyroid and had 15 years of painful muscles and joints and fatigue. My blood tests show B5 and B12 are high but I am always anemic at the same time due to malabsorption. Recently my Dr suggested cutting gluten and put me on low dose Predisnolone. All the pain is gone, I move like I am 20 years younger and have had 6 different people comment on how different I look. I have been pretty much gluten/ wheat and oat free but slipped up a couple of times and noticed symptoms of bloating, nausea and constipation almost immediately. I never gave it much credence because I didn’t want to give up bread etc.. before but now there is no going back. Try going GF and see if it works for you.
Maggie, contact me maybe I can help. stikovicm@gmail.com
Just wanted to mention that B12 tablets and vitamin E can help a lot, but take the iron and Vitamin E 8 hours apart for better absorbtion.
is iron loss only associated with blood loss or are there other situations which cause low iron
family members have been dealing with low iron for a while – and are at a loss for recovery
i ask these questions because there seems no agreement from one doctor to another – both sides
claim their opinions are the truth
if any of your readers [or you yourself] could give some insight – it would be appreciated
Interesting article. Just wanted to know if the ultra iron supplements have soy in them as I can’t have any.
Hi Alicia,
No Soy in our Ultra Iron 😉
All the best,
Dr. O
I have been anemic for the past 15 years not knowing what caused the iron deficiency till recently when a doctor told me that I am allergic to cereal. I take iron supplements throughout to keep my blood level close to normal but without it, then few months of menses will bring it down to very low levels. On the other hand, I have acne, and another doctor said its iron deficiency related. How can I manage a gluten free life to deal with these to problems, iron deficiency and acne?
Hi I’m from Australia. For over 15 years I had a chronic cough and mountains of mucous, went to doctor after doctor. I would vomit after some meals. No doctor ever suggested that I had a gluten tolerance issue. It was trial and error that I finally found out it was gluten. Also for 17 years now I have had an iron deficiency and couldn’t understand why until the other day finally a specialist diabetic doctor asked if I had a gluten intolerance and told me about the low iron absorption issue because of gluten finally an answer. Don’t know yet if my iron levels will improve, I hope so. Thank the Lord for the internet.
I was anemic, diahrea etc and endoscopy showed villi blunting. Blood test negative for ceoliac. Went gluten free, took oral iron to sort out anemia. Felt better, blood tests normalised for short while then chronic abdomen pain . 2nd endoscopy showed normal Villi but biopsy showed non specific chronic gastritis and duodenitis. Bad reaction to PPI. Felt fatigued again. Went for another blood test, deficient in iron and vitamin d but thankfully not anemic.Referred to dietician to try and sort out if l am eating gluten accidentally or another intolerance/ cause.
I am replying to myself as l thought it would be useful to have an update. Interesting talk with doctor. Am totally gluten free, diagnosed gluten intolerant/ not ceoliac as negative blood, although villi damage. Have continued to have stomach pain , sore bruised feeling most days. Now having reflux more often, ( new symptom.) I have been wondering if other food intolerances are the cause as well if symptoms continue. Also doctor said low stomach acid could be a potential cause .That can cause a load of problems, and PPI makes it worse. I just feel it’s never ending, l think gluten has alot to answer for, l think it has irritated my stomach and duodenum so that l developed the chronic gastritis and duodenitis. Any help appreciated!! Fed up, l don’t want to mask my symptoms with painkillers.
Three weeks ago I was diagnosed at level 4 of iron. Very low. I asked to get tested for gluten intolerance and the result was negative. I am taking supplement now and will get tested next month. I am eating gluten free. The one difference from eating gluten free is that I am not gassy nor bloated. The iron pills are helping as energy level is up. Even if the one blood test for gluten free came out negative, I could still be gluten intolerant?
Diana,
Yes,
Blood tests are notorious for false negatives as it relates to gluten sensitivity. Especially non celiac gluten sensitivity. That’s why we recommend genetic screening to identify the genes.
Hope you get it figured out!
Dr. O
Where do you go for genetic screening? And how do one test for gluten sensitivity?
Catherine – you can do genetic screening here – https://stg-gfsociety-testing.kinsta.cloud/genetic-testing-for-gluten-sensitivity/
This is such an interesting site! For the past 10 to 15 years I have struggled with anemia. I had to take iron tablets even though I ate plenty of meat, for some reason I wasn’t absorbing iron properly. I had colonoscopies endoscopy’s, Etc. I finally change doctors she sent me to a pathologist oncologist. This doctor said that my platelets had kept increasing and increasing and increasing due to the fact that my body was not absorbing iron and could not make enough red blood cells. She wanted me to start taking iron infusions, of which I had a severe allergic reaction to and ended up with other problems. She did a gluten test which was negative but I found out later that since I had not been eating gluten for three months it wouldn’t show anything anyway. It was then assumed that I should stay away from any type of greens beans etc. since this time, i’ve began eating mostly meat with very few vegetables occasionally. I now do not have sinus issues, I have clear skin, I have energy, and I have lost approximately 70 pounds. My BMI is 25 for the first time in years. I am no longer constipated, And my life is completely better. I wish I had done this decades ago.
So wonderful to hear your story of success Julia!
Thanks for sharing!
All the best,
Dr. O
These are my latest results. My ferritin level went from 17.2 on 1/13/202
To 140.2 on 12/8/2020.
Why was it assumed that you should stay away from greens/beans? Do you think that helped with the ferritin or just going gluten free did? Thanks!
I am trying gluten free ONLY, but so far no results, ferritin is still getting lower.
Can you please assist me, I m having same issues of low iron, even iron pills are not helping to increase my ferritin levels, it is been more than 2 years. I am on gluten free diet from last 2 months, and my ferritin went from 35 to 20 in this month. Please suggest what should I do? And what it that removing Greens beans etc from food?
Did your iron improve?
I’m having same issues, low and low iron…started gluten free and still going lower, ferritin is 11, and even iron supplement did not help instead gave me many other health issues.
My entire life I’ve suffered with severe heart burn and constipation and asthma. Last October my ferritin level was 5, this was the first time blood tests showed iron deficient anemia. I was given 2 iron infusions. Egd showed gastritis, capsule for small intestines showed erosions and a MVA. When asked if if I had celiac disease was informed no. I feel angry and a little stupid. My GI doctor has given me a total of 3 egd and 3 colonoscopies. Dx with Barrett’s and gerd. Put on ppi and iron. I read that ppi (proton pump inhibitors) can actually cause iron deficiency. I decided to stop taking them and looked into what to stop eating to decrease heartburn as it has been severe my whole life and the ppi had been a god send, so I thought.
I read to stop eating gluten to see if this might be the problem. I haven’t had heartburn, constipation or allergy symptoms ever since. I’m 62 years old, a registered nurse and I just can’t believe this is what has been torturing me my entire life and I always had the power to stop it. I have seen gi doctors, Ent, allergists, internists, primary Md. They always had a lot to say however none of them ever suggested to try this one simple thing. Free at last
Amazing story Kathleen! Sorry you had to go through all of that to get an answer, but excited that you finally found one.
Thanks for sharing with us!
All the best,
Dr. O
I have been dealing with the bloating (look 9 months pregnant after eating), breathing problems, etc etc for years. I just recently tested for gluten, celiac and had my iron and ferritin checked. A major revelation happened when my natropath had me checked for the MTHFR gene mutation…..2 copies, making me homozygous…..big piece of the puzzle!! Look into it!!