new to the gluten free journey?
new to the gluten free journey?

Contents
Toggle
Stay up-to-date with the latest articles, tips, recipes and more.

*These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure or prevent any disease.
If you are pregnant, nursing, taking medication, or have a medical condition, consult your physician before using this product.
The entire contents of this website are based upon the opinions of Peter Osborne, unless otherwise noted. Individual articles are based upon the opinions of the respective author, who retains copyright as marked. The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Peter Osborne and his community. Peter Osborne encourages you to make your own health care decisions based upon your research and in partnership with a qualified health care professional.
7 Responses
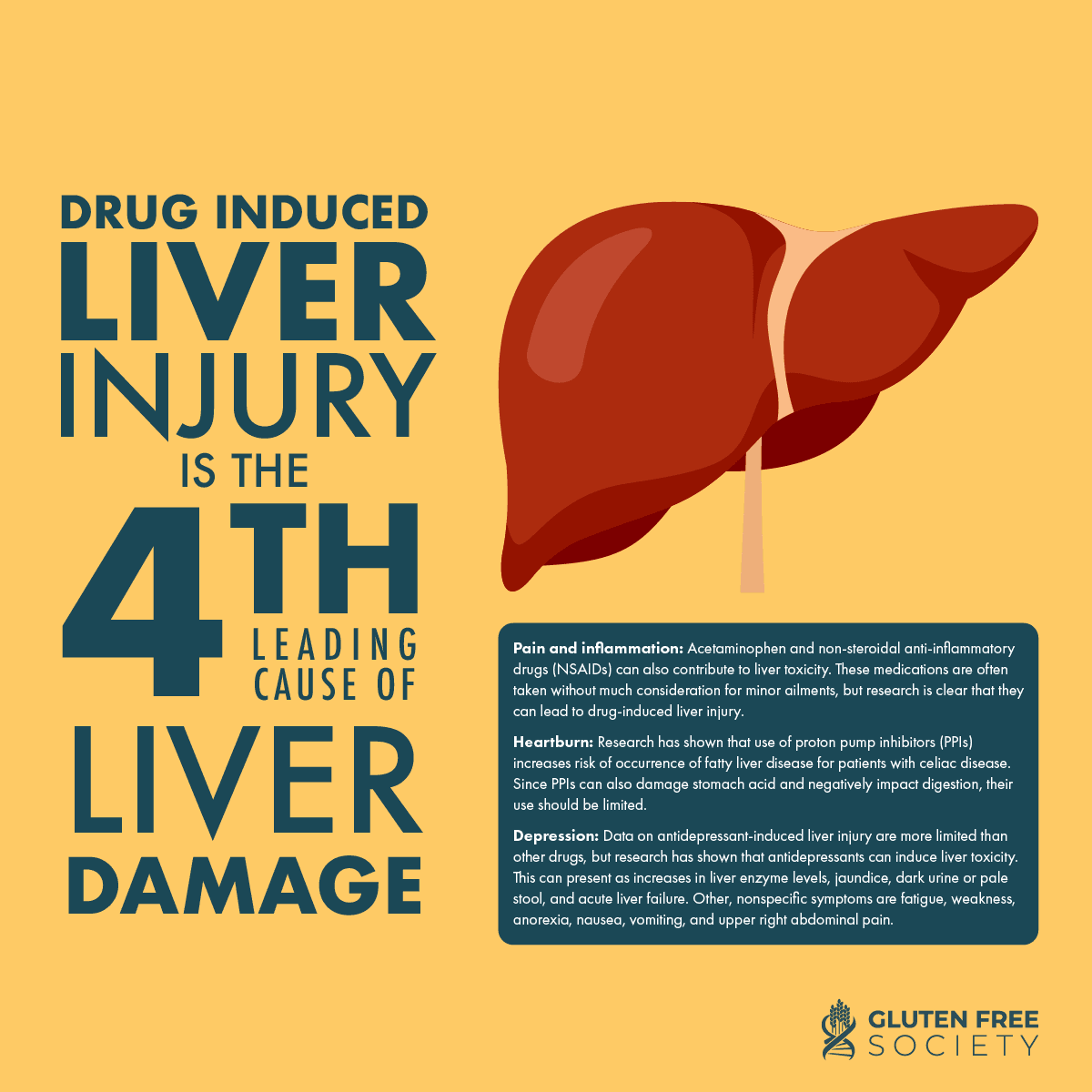
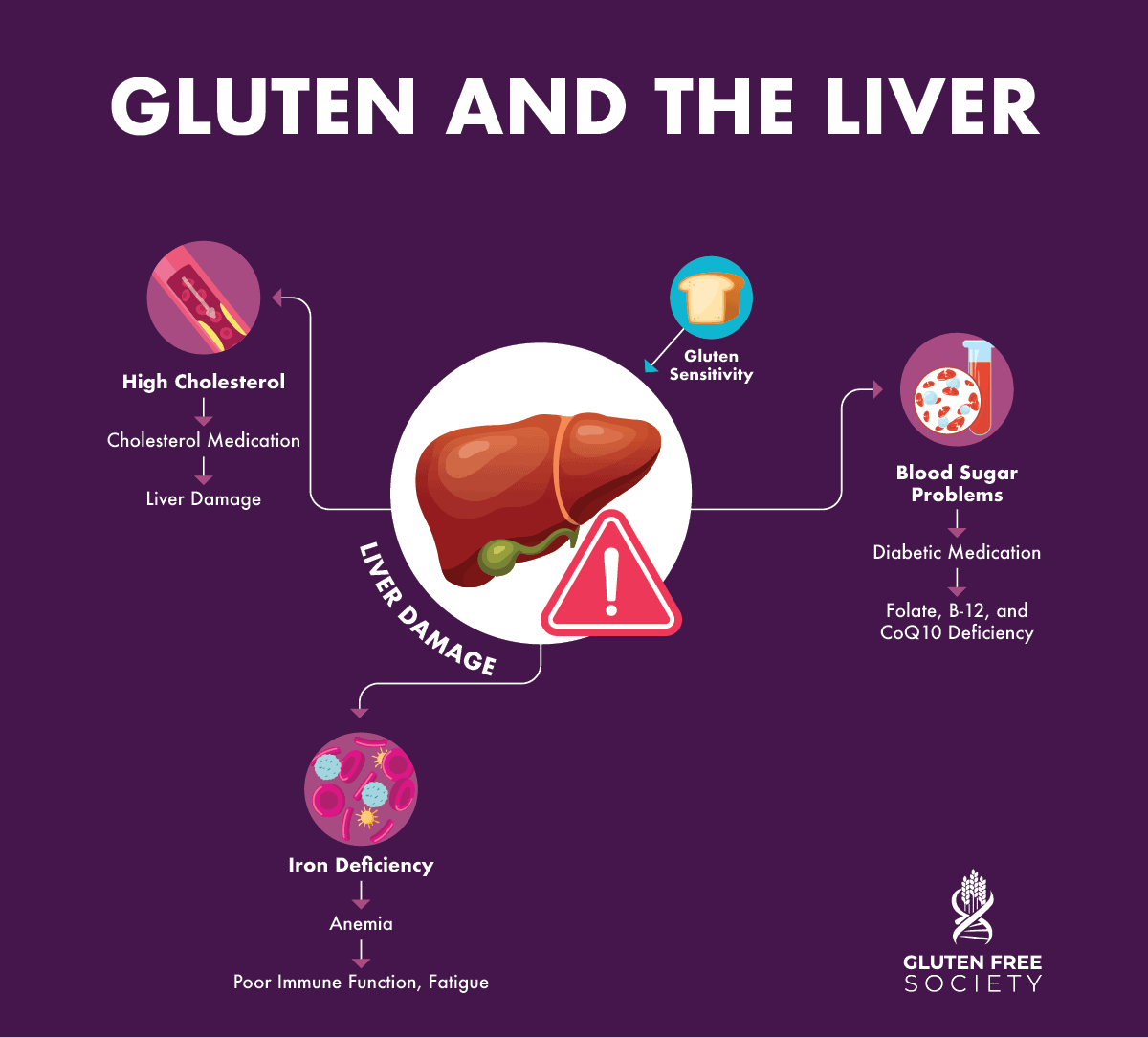
Suddenly, my front teeth are turning black! I do have leaky gut and advanced liver disease with inflammation throughout my body that’s barely tolerable. I wonder if a detox will be too stressful for my liver?
ever tried LDN?
I do wish everyone would stop using abbreviation. Some of us have no idea what they mean. What is LDN? Thank you.
LDN is low dose naltexone from a pharmacy.
How do you test for yeast issues?
I do have coeliac gene and Hashimoto’s gene was diagnosed with this condition in my later years and know I suffer from chronic lymphatic inflammation and sibo caused by miss diagnosed im having lots of health problems because of late discovery my teeth are really bad from all you know the risks thanks for your great information it’s helpful for me to understand better
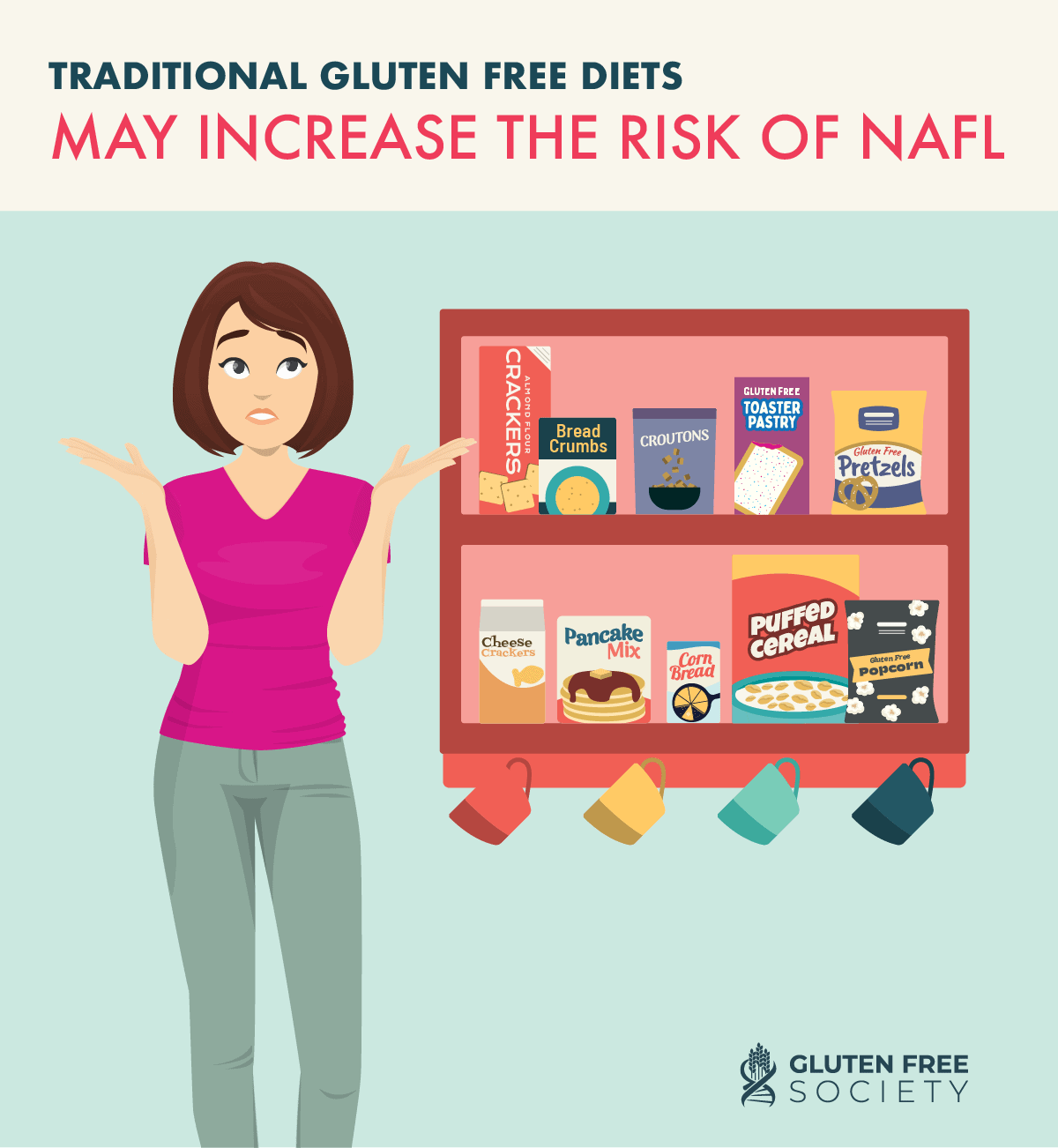
My son has NAFLD and now he has Cirrhosis. Are there any supplements he can take to get off the steroids safely so his liver can work more optimally? He’s living with his brother who is my youngest son. I’m freaking out because I’m still going through testing. I have not been shown to have HLA DQ2 OR 8, but I have HLA DQA1*05 but they didn’t test me for HLA DQB1*02. I read that if I have that heterodimer that it is just like having HLA DQ2.5. IS this true. can my sons have Celiac and had it their whole lives and gone undiagnosed? I need help!!