Is Gluten a Brain and Nerve Toxin?
Heard of Leaky Brain? We know that gluten can contribute to a wide range of complications within the body. Yes, digestion is the most common, but celiac disease and gluten can affect everything from oral health to gut health. But can its effects extend all the way to the brain? Incredibly, yes. Our body’s systems don’t work in isolation. They are all interconnected and one root problem can cascade into a range of reactions throughout the body. Such is the case with gluten. Lets dive in to how gluten affects the brain.
When it comes to the brain, there are two mechanisms by which gluten can impact brain function. First, it can compromise the blood brain barrier – a critical layer that protects the brain from harmful substances. This condition is called Leaky Brain. Second, gluten-induced nutritional deficiencies can contribute to neurological problems and also impair their repair and healing. This article focuses on these two ways in which gluten can influence brain and nerve health, and the many downstream effects that compromised brain and nerve function can impact the body.
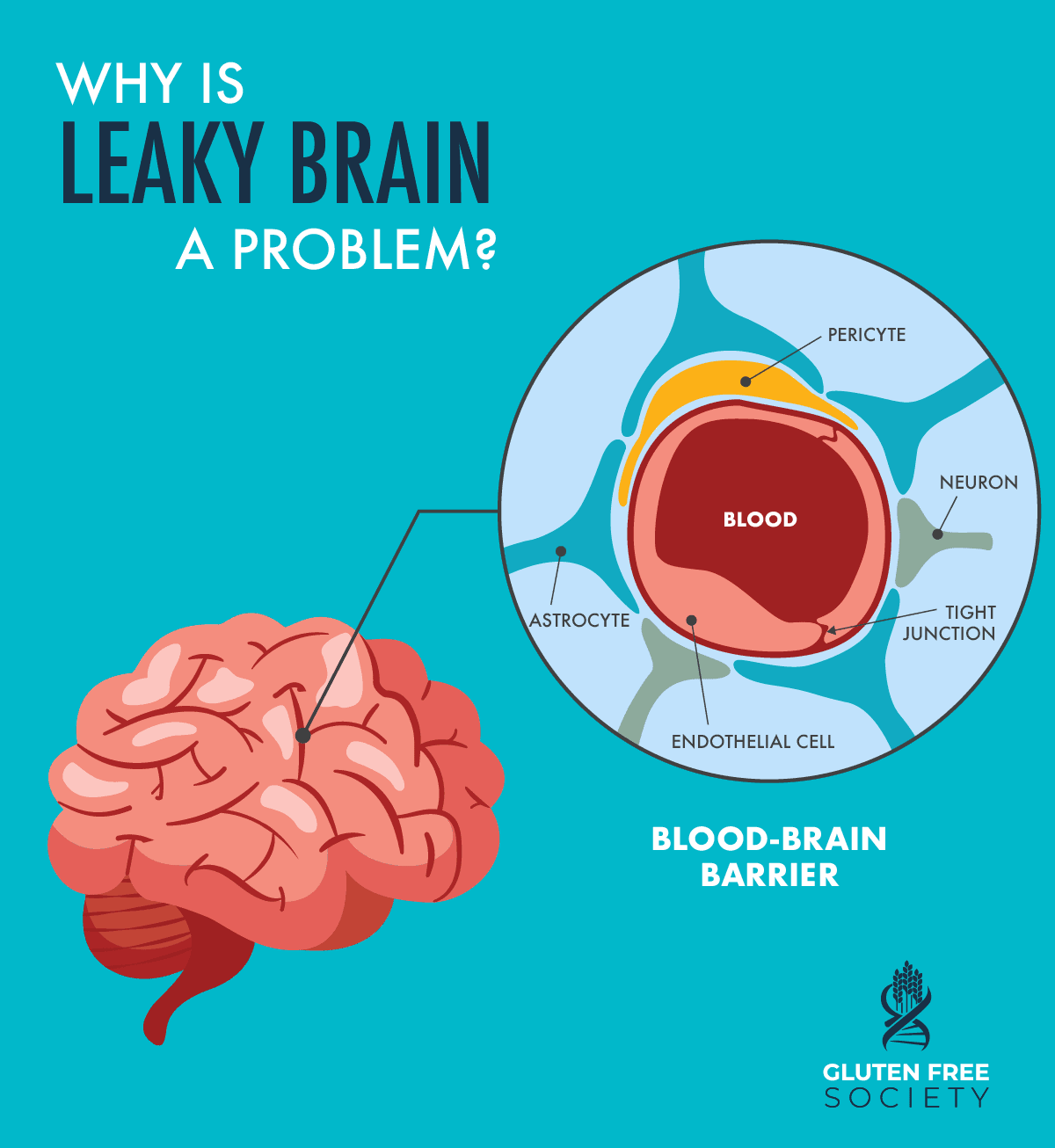
What is Leaky Brain?
First, let’s discuss a bit more what Leaky Brain even means. We’ll then get into how Leaky Brain can cause complications within the brain and nervous system to contribute to a wide range of related health issues.
Just like gluten can contribute to intestinal inflammation and permeability, or
leaky gut, it can also contribute to Leaky Brain.
Research has shown evidence that patients with gluten and dairy reactions have antibodies showing up in their cerebrospinal fluid. Antibodies are proteins made in response to infections, and so the presence of antibodies means that the body has made efforts to fight off a specific infection. In the case of leaky brain, antibodies are an indicator that a disruption in the blood brain barrier is present.
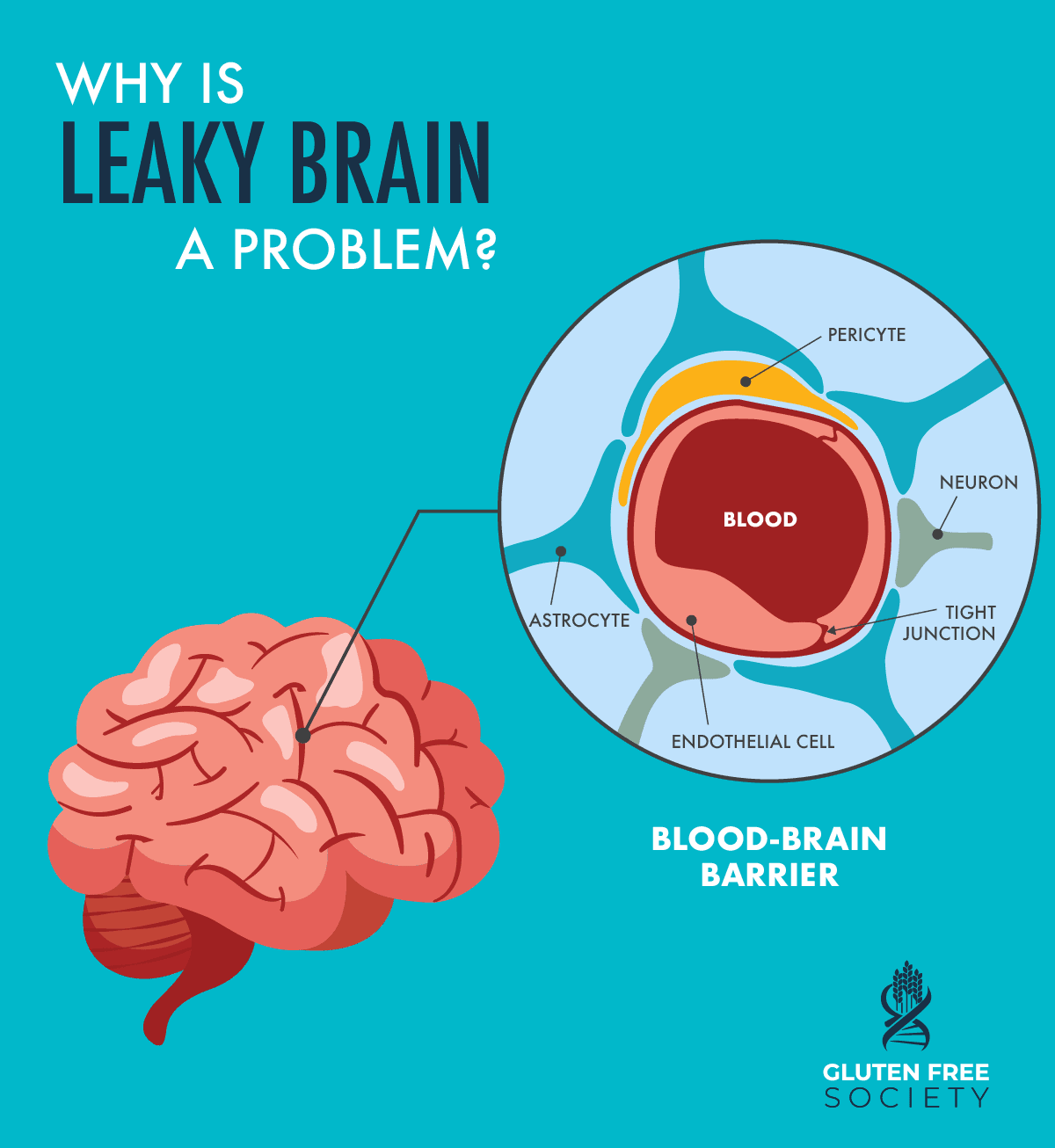
Why is Leaky Brain a Problem?
Why is leaky brain a problem? Well, really the same reason a leak in anything is a problem. The “leak” in Leaky Brain refers to a compromise in the blood brain barrier. Similar to how the barrier in the gut prevents toxins from passing through, the barrier in the brain (the blood brain barrier) prevents elements in the circulating blood from crossing into the fluid of the central nervous system where important neurons exist.
You can think of it like this: the skull helps protect the brain against physical damage and the blood-brain barrier protects against disease-causing pathogens and toxins that may be present in our blood. If this barrier becomes leaky, it opens up the potential for a number of health problems, from inflammation to infection.
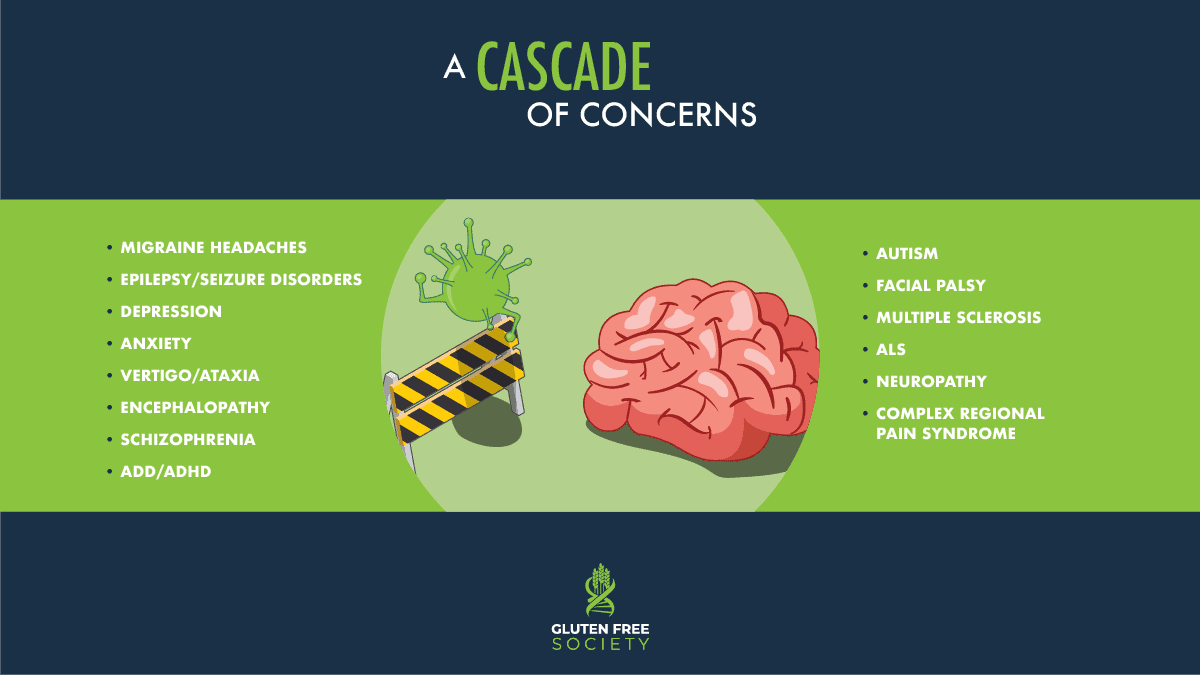
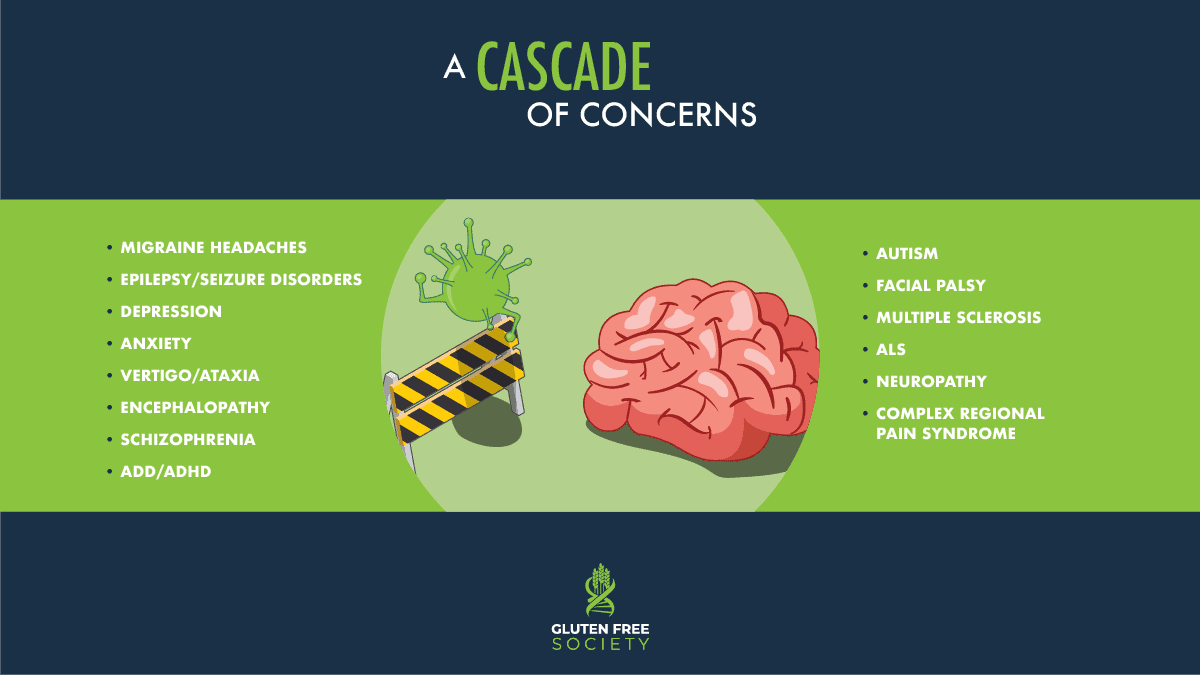
Gluten Causes Damage to the Brain & Nerves in a Variety of Ways
These problems can then lead to further complications that impact the central nervous system – diseases stemming from brain and neurological inflammation, to autoimmunity, and a barrage of nervous system disorders. In fact,
some research estimates that gluten intolerance can be associated with central or peripheral nervous system and psychiatric disorders in a significant proportion (10–15%) of cases.
Further research has suggested that a strict gluten-free diet is an effective first-line treatment of the neurological manifestations of gluten-related disorders. Below are several potential complications of leaky brain:
- Migraine Headaches: When the gut-brain axis is disrupted, neurotoxins can leak into your brain and cause inflammation. These neurotoxins can include lipopolysaccharide (LPS) endotoxins, inflammatory cytokines, food antigens, chemicals, histamine, and nitric oxide. The brain inflammation they cause can trigger migraines. Additionally, researchers have identified gluten as a possible trigger for migraine headaches, and suggest that a gluten-free diet may help alleviate headache pain in those with celiac disease or gluten sensitivity.
- Epilepsy/Seizure Disorders: Leaky brain is associated with an increase in the chemical messenger glutamate, has been suggested in the process of developing epilepsy. Not only does it contribute to the development of epilepsy, it is also thought to affect the effectiveness of and resistance to anti-seizure drugs due to the influx of serum proteins that can bind to drugs and reduce their effectiveness in the brain. This connection has been studied by the Epilepsy Foundation. In addition, gluten sensitivity has been linked to epilepsy directly. Multiple studies have shown the benefit of the gluten free diet in patients with seizures.
- Depression: Depression and related mood disorders are reported to be associated with gluten sensitivity and celiac disease. Research suggests one possible cause of this connection is leaky brain, which can be triggered by gluten and causes elevated peripheral pro-inflammatory cytokines.
- Anxiety: Various types of anxiety are associated with both leaky brain and gluten intolerance. One study found that celiac disease patients were significantly more likely to have anxiety when compared to controls, and that after one year on a gluten-free diet, there was a significant improvement in anxiety symptoms. In fact, some research even suggests that a gluten-free diet may positively influence mood in subjects without gluten-related disorders.
- Vertigo/Ataxia: The effects of leaky brain can also contribute to vertigo/ataxia. Multiple research studies have found that adherence to a strict gluten-free diet could help improve the symptoms of vertigo/ataxia.
- Encephalopathy: Encephalopathy is a general term describing a disease that affects the function or structure of your brain. There are many types of encephalopathy and brain disease, but the integrity of the blood-brain barrier has been cited in research as a common root cause of various types of the disease.
- Schizophrenia: a wide body of research suggests that Schizophrenia may be the psychiatric disorder with the most robust relationship to celiac disease. Additional research suggests this relationship may be driven by the inflammation and immune response that exists in a leaky brain condition.
- ADD/ADHD: The inflammation and immune response characteristic of leaky brain can contribute to attention-related brain complications as well, including ADD and ADHD. Studies have shown that many diagnosed with ADD/ADHD show remarkable improvements when following a gluten free diet.
- Autism: Research has shown that there is an altered expression of genes in the brains of those with autism that is associated with blood-brain barrier integrity. This is coupled with increased neuroinflammation and possibly impaired gut barrier integrity. A growing body of research shows that gluten free diets can play a role in the improvement of symptoms for those diagnosed with autism.
- Facial Palsy: Facial palsy or weakness of facial muscles is another manifestation of neurological conditions. One study of acute peripheral facial palsy found that approximately one-third of participants had a compromised blood-brain barrier. In addition, research has linked gluten as a possible cause of facial palsy.
- Multiple Sclerosis: Multiple sclerosis (MS) is generally considered an inflammatory disease leading to tissue injury within the central nervous system. In affected areas, the blood-brain barrier becomes leaky and allows the entry of serum proteins and cells into the central nervous system. Researchers have linked gluten as a trigger for the development of MS.
- ALS (Amyotrophic Lateral Sclerosis): ALS, or Lou Gehrig’s disease, is a progressive nervous system disease that affects nerve cells in the brain and spinal cord, causing loss of muscle control. One case evaluated brain imaging and found ALS improved after the institution of a gluten-free diet.
- Neuropathy: Comprehensive research provides evidence on the substantially increased risk of neuropathy in patients with celiac disease, and indicates that adherence to a gluten free diet appears to improve symptoms of neuropathy. The relationship between leaky gut, leaky brain, and neuropathy has been studied as a compelling connection to celiac disease.
- Complex Regional Pain Syndrome (also known as Reflex Sympathetic Dystrophy): Complex Regional Pain Syndrome (CRPS) is characterized by pain in combination with sensory, autonomic, and motor symptoms that may include weakness, tremor, myoclonus and dystonia of the affected limb or limbs. CRPS often originates from tissue injury but accumulating evidence suggests that CRPS may involve both autoinflammatory and autoimmune components. Additionally, CRPS shares a similar genetic pattern with celiac disease, as both conditions are more likely when someone has an HLA-DQ8 genotype.
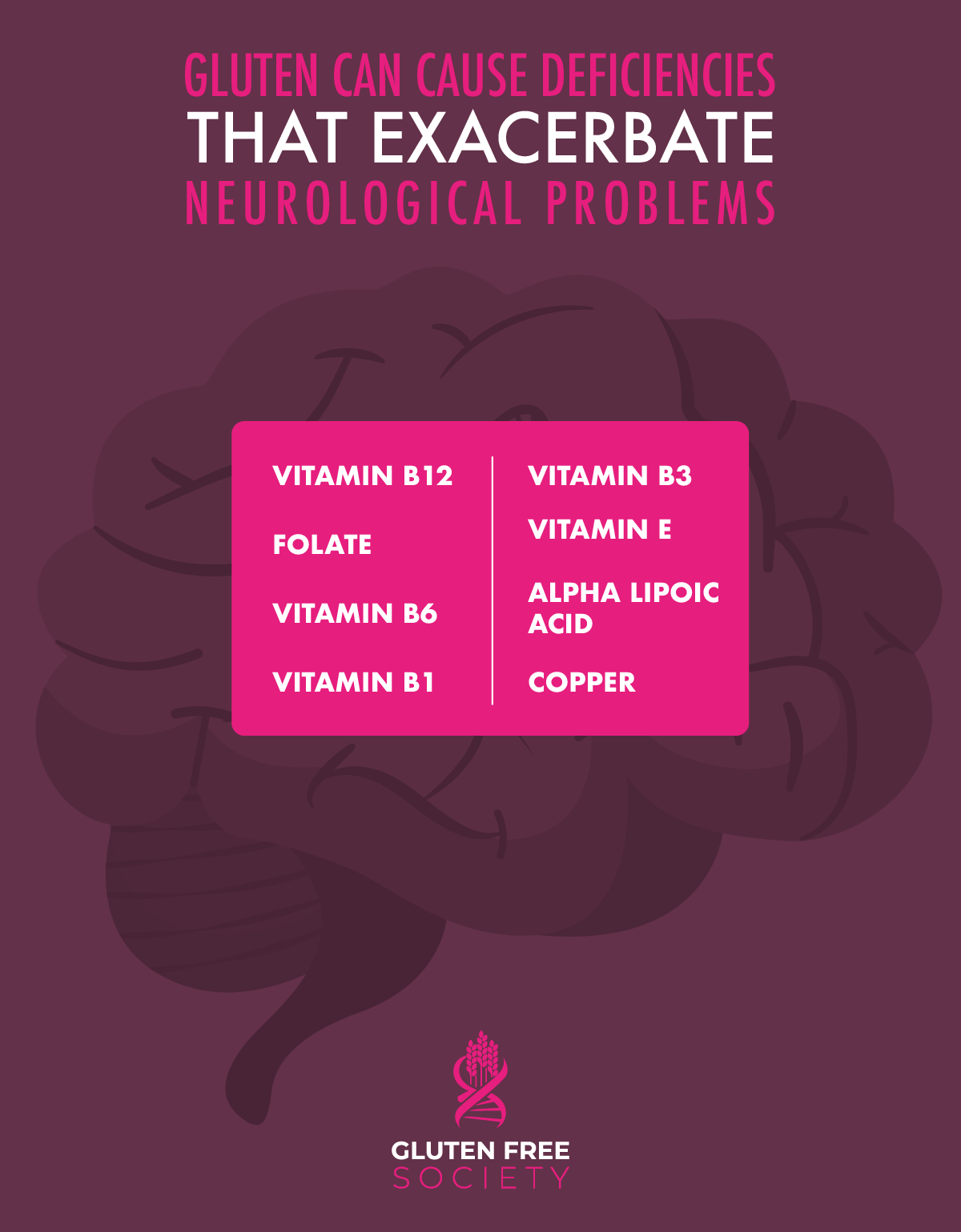
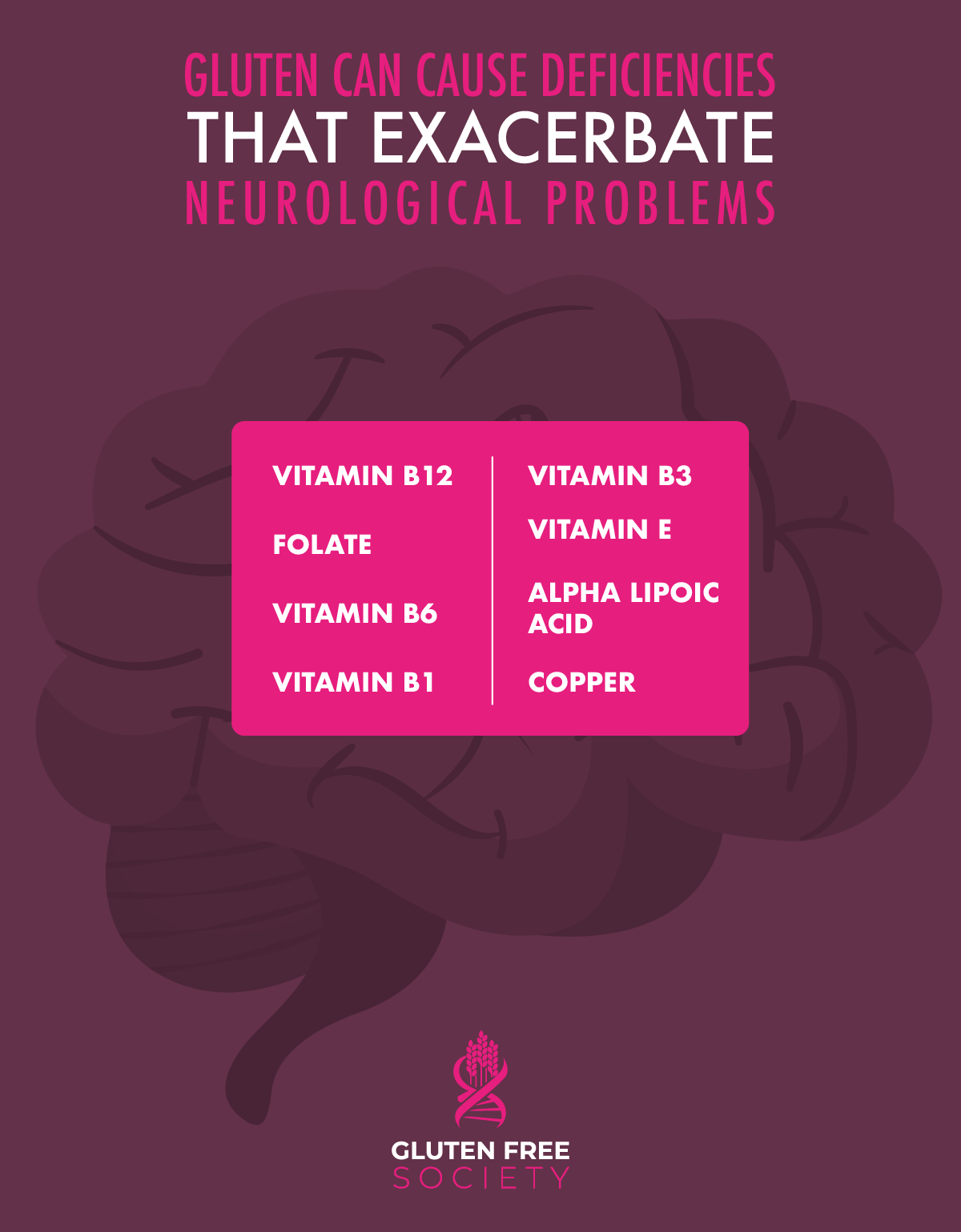
Gluten Induced Nutritional Deficiencies Exacerbate Neurological Problems
But gluten doesn’t just influence brain and neurological health through leaky brain and autoimmune inflammation, it can also contribute to nutritional deficiencies which then
cause or exacerbate neurological problems. Nutritional deficiencies caused by gluten consumption and its damage to the intestines can also impair the repair and healing of neurological problems.
- Vitamin B12: Absorption of vitamin B12 is impaired in those with celiac disease. Vitamin B12 deficiency can impair both upper and lower motor neuron dysfunction (sometimes appearing as decreased reflexes). It is also associated with cognitive dysfunction and can contribute to megaloblastic anemia.
- Folate: The absorption of folate, or vitamin B9, like most B vitamins, is impaired in those with celiac disease. The neurologic manifestations of folate deficiency are quite similar to those of vitamin B12 deficiency. They typically include cognitive impairment, dementia, depression, and, less commonly, peripheral neuropathy and subacute combined degeneration of the spinal cord.
- Vitamin B6: Vitamin B6 deficiency can result from malnutrition or malabsorption, as is the case in celiac disease. Vitamin B6 deficiency can present in all ages. In infants, vitamin B6 deficiency is a cause of seizures. In adults, neuropathy due to vitamin B6 deficiency involves numbness, paresthesias, or burning pain. These sensations typically begin in the feet and then ascend to the legs and hands.
- Vitamin B1: Vitamin B1 or thiamine deficiency can occur due to malnutrition or malabsorption. It often presents first as neuropathic symptoms (numbness, tingling, pain, or weakness) and then progresses to cognitive symptoms. It may also involve complications with cranial nerves, like tongue, facial, and laryngeal weakness.
- Vitamin B3: Niacin or vitamin B3 is absorbed in the intestine and therefore those with celiac disease are at risk of deficiency. The most common manifestation of vitamin B3 deficiency is a condition called pellagra. The classic presentation of pellagra involves dermatitis, dementia, and diarrhea.
- Vitamin E: Most vitamin E deficiencies occur in patients with malabsorption or transport deficiencies, including celiac disease. Vitamin E is an antioxidant and a free radical scavenger, and so the neurological manifestations of vitamin E deficiency are primarily related to the loss of this protective function. Manifestations include pigmented retinopathy, loss of vibration and proprioception, loss of deep tendon reflexes, ataxia and cerebellar degeneration as well as generalized muscle weakness
- Alpha Lipoic Acid: Alpha Lipoic Acid acts as an antioxidant that is easily depleted in those with celiac disease. It’s protective properties have shown promise against cognitive decline as well as diabetic neuropathies. In fact, one study found that supplementation with Omega-3 fatty acids plus Alpha Lipoic Acid slowed cognitive and functional decline in patients with Alzheimer’s Disease over a 12 month period. These benefits were not observed with Omega-3 supplementation alone.
- Copper: Copper is absorbed in the stomach and small bowel, and celiac disease has been associated with copper deficiency. Copper deficiency often presents in a way similar to vitamin B12 deficiency and may result in myeloneuropathy – the simultaneous damage of the tracts of the spinal cord and peripheral nerves in the lower limbs.
Identifying the root cause of gluten consumption and/or celiac disease can help the body heal from nutritional deficiencies as well as many of the potential diseases that can result. A first step in healing is to identify and correct any existing nutritional deficiencies. This can be done through testing with a qualified practitioner who is well-versed in the implications of nutrient deficiencies and celiac disease.
Conclusion
Even though the gut and brain may seem quite independent, the reality is, nothing in the body works in isolation. If brain and neurological symptoms are a concern, it is worth investigating and ruling in or out whether celiac disease or gluten consumption could be at the root of your problems.

2 Responses
Thank you for this information. It confirms much of what I have independently concluded through the “school of hard knocks”. I have suffered from trigeminal neuralgia for over 20 years and I don’t feel surgery is the answer for me. I am convinced there is a reason that it gets better and worse at times. I am on a gluten free diet, but have not eliminated all grains. I would welcome any experiences that others have had.
MY celiac disease was diagnosed about 20 years agohowever I still have neurological symptoms so I’m trying to repair my body with vitamins, protein powders like spiraling, hemp, an I section every 6 weeks called Myers cocktail containing B vitamins, calcium, mag rsium and vit c. I cook all my own food, vegetable soups, stews and fish, no grains or cereals of any kind. I take 2 drops daily liquid selenium to facilitate hormone exchange of my hypothyroidism. I have improved a lot but am not normal. Think i have sustained too much damaged during years of doctors unable to diagnose celiac. Wish you well.