Perhaps you’ve heard the phrase cross contamination. It’s commonly used in reference to food contamination with bacteria, for example, not using a clean cutting board to cut vegetables after cutting raw chicken. This type of cross contamination in a cooking space can put you at risk of foodborne illness or food poisoning.
But there is another type of cross contamination that is important for those of us who avoid gluten: gluten cross contamination. Gluten cross-contamination happens when gluten free food comes into contact with food containing gluten or cooking utensils and surfaces that have been used to prepare it. It is unfortunately quite common in high volume food preparation areas like restaurants and commercial food processing or packaging facilities.
Causes of Gluten Cross Contamination
With the popularity of the gluten-free diet rising, an increasing number of food manufacturers and restaurants are attempting to provide gluten free options. However, as food manufacturers and restaurants work quickly to adapt to changing demands to capture their share of the gluten-free market, they often don’t take the time and care needed to ensure that their changes in processes and ingredients are comprehensive, safe, and truly gluten-free.
FOOD PRODUCTION
In food production, cross contamination can happen as part of the manufacturing process or the packaging process. Cross contamination can be a result of contaminated equipment, or a facility employee who did not take proper precautions between producing or packaging a gluten-containing food and a gluten-free food.
For example, if a gluten-containing product is manufactured before a gluten-free product and the shared production lines are not thoroughly cleaned between products, trace amounts of gluten can get into your food. You may see labels on some products stating that it was made in a facility that shares equipment with products containing other allergens, like wheat or gluten.
For this reason, you may choose to seek out only products that were produced in a gluten-free facility (this can be hard to verify, but you can contact the company directly to ask), or that have been tested after production to earn a
Certified Gluten-Free label.
RESTAURANTS
Eating out at restaurants is one of the most common areas where cross contamination occurs. This is because it is virtually impossible to ensure that all staff members are trained appropriately to understand the care that must be taken to keep food free of gluten. There are a number of ways that food can become contaminated in restaurants.

People to Food Gluten Contamination
This happens when a restaurant worker touches food containing gluten, for example, a piece of bread put on the side of a salad, and then without washing hands or changing gloves, touches food for your well-intentioned gluten-free meal.
Food to Food Gluten Contamination
This happens when gluten from one food contaminates an otherwise gluten-free food. A common place where this happens is in deep fryers that are used to fry all food together (for example, chicken fingers on a kid’s menu and seemingly gluten-free truffle fries for an adult side dish).
Equipment to Food Gluten eContamination
This happens most often when a restaurant does not have a dedicated gluten-free kitchen, or gluten-free area of their kitchen. They may use a shared grill, cutting board, skillet, or utensil for both gluten-free and gluten-containing foods. For example, your grilled chicken may be on the same grill as a bun being toasted, with one spatula being used to lift both onto plates.
Cross Contamination of Processed Food
In addition to cross contamination of gluten-free foods in both home and commercial food production areas as well as restaurant environments, research has shown that even processed food that is labeled gluten-free or that doesn’t explicitly list any gluten-containing ingredients can also pose a possible risk.
For example,
one study conducted in Gluten Free Watchdog and reported in Reuters tested 101 foods sold in the United States that didn’t include ingredients known to contain gluten. Fourteen of these items did include allergy advisory statements for potentially containing wheat or gluten on the label and one of those 14 tested positive for gluten. Among the 87 products without allergy advisories, 74 contained little or no gluten, nine contained gluten in amounts ranging from at least 5 ppm but less than 20 ppm, and four foods had at least 20 ppm of gluten. For reference, U.S. Food and Drug Administration guidelines require packaged foods labeled “gluten-free” to contain less than 20 parts per million (ppm) of gluten.
In addition, a
study published in Biomed Central Gastroenterology confirms that avoiding even “gluten-free” processed foods improves healing in those who have previously gone traditionally gluten free and not responded (this is often referred to as non responsive disease). The study evaluated the effects of a 3-6 month diet of whole, unprocessed foods, termed the Gluten Contamination Elimination Diet (GCED), on NRCD. Prior to the GCED, all patients were interviewed by an experienced dietitian and no sources of hidden gluten ingestion were identified. The study found that 82% of those who did not respond to a traditional gluten free diet made a full recovery by eliminating processed food. A more robust summary of the study can be found
here.
The takeaway here is that again, healthy whole foods like vegetables, fruits, nuts, seeds, and pastured meats and eggs are the safest (and most nutritious) option for a gluten-free diet.
How to Prevent Cross Contamination
At Home
Cross contamination at home occurs most frequently in homes that include some people who eat gluten and some gluten-free eaters. It also occurs frequently soon after a new diagnosis.
In mixed homes (gluten-eaters and gluten-free-ers)
When some people in the house continue to eat gluten, they may not be cautious about containing their gluten-containing food, and may contaminate shared surfaces, condiments, and equipment. It is important to educate all members of a household on the importance of keeping surfaces clean of gluten, and to separate certain condiments and appliances that cannot be properly cleaned between uses.
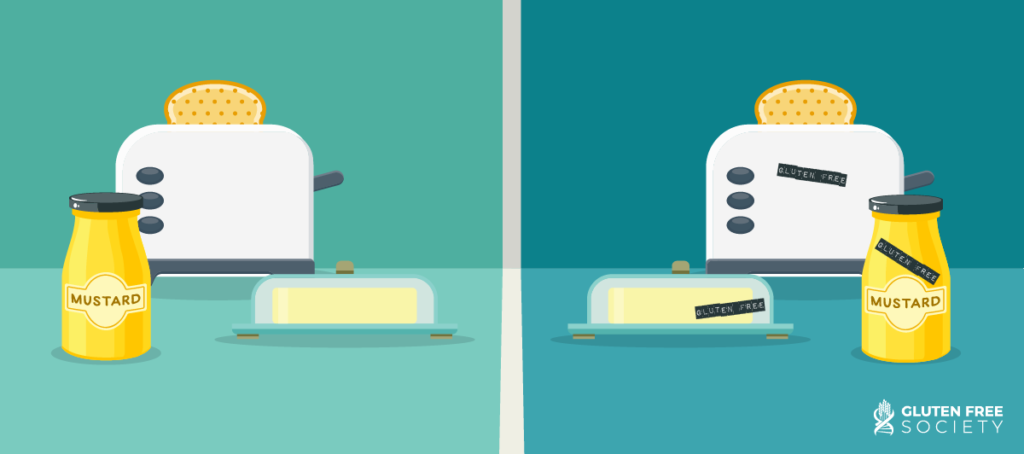
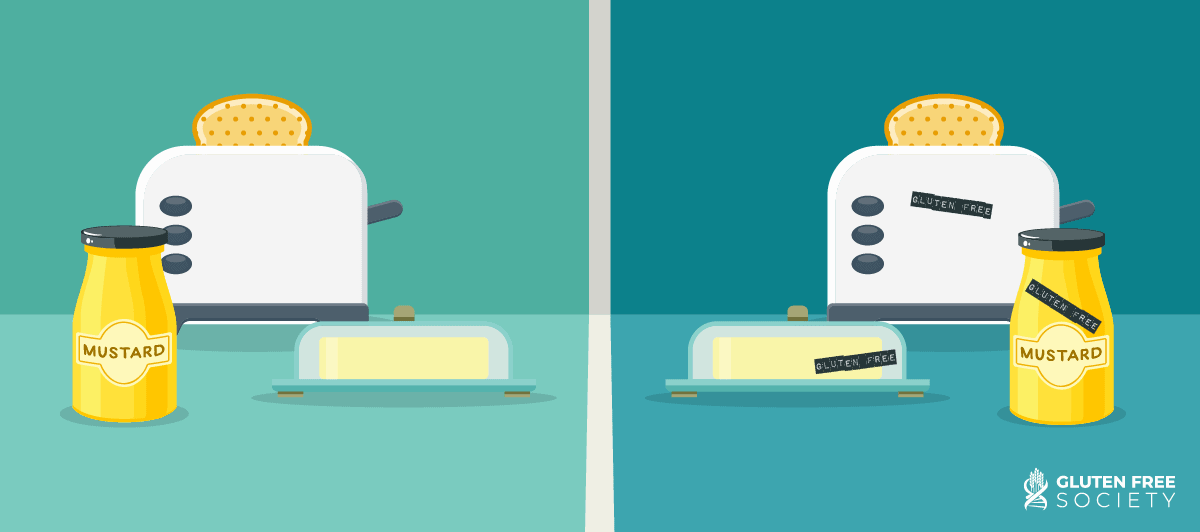
If used by both gluten-eaters and gluten-free-eaters, I recommend getting separate small appliances like toasters that may harbor crumbs that cannot be cleaned. I also recommend always having separate condiments that require you to dip into a shared container, like a jar of mustard or a butter dish. In addition, dedicating only one area of your kitchen as the “gluten counter” or “gluten space” can help contain gluten and prevent cross contamination.
If other household members or guests have gluten at the same meal as you (for example, bread or rolls at dinner), keep them off the table, only in the gluten area of the kitchen. If serving family style, have other members fill their plates first with gluten-free food and then visit the gluten area to get gluten-containing food. When getting second helpings, it’s wise to get a new plate. Get everyone in the habit of washing hands both before and after meals. Finally, be sure to read the tips below for transitioning your home to be gluten-free, as some of these same sources of cross-contamination will still apply.
In dedicated gluten-free homes
If you’re lucky enough to live in a home where you can transition to be entirely gluten-free, your risk of cross-contamination will decrease tremendously. However, making the transition can be a bit tricky, as there are likely sources of contamination throughout your kitchen.
Think about all of the places that gluten may have touched. These may include small appliances like toasters or toaster ovens, your knife block, your jars of spices or baking supplies (we often use a measuring cup or spoon to dip first into flour and then into sugar), any condiments, and built in cutting boards or blocks. All of these items should be replaced when making the transition. If in doubt, toss it out!
When Eating Out
As a general rule of thumb, I recommend avoiding eating out as much as possible since it is impossible to control the potential for exposure. However, I realize that this isn’t often feasible, so here are some tips for when you do eat out:
- Seek out gluten-free or health-focused restaurants: Dedicated gluten-free restaurants aren’t too common, but they are popping up more and more, especially in major metropolitan areas. Take some time to do a bit of online research to see if any exist in your area, or in the area you’ll be visiting. As a next-best option, seek out health-focused restaurants. While they may serve gluten, their staff is generally more conscientious of dietary restrictions and more likely to take the care needed to ensure your meal is actually gluten-free than, say, a pizza place that happens to offer a gluten-free crust. The app Find Me Gluten Free can be a helpful resource in doing some research in advance. However, most of the content is user-generated, so don’t put too much trust in another person’s review – do your own research too. And be aware that the information from this app may also include corn, rice, oat, and other grain based ingredients that could be problematic for your gluten free diet.
- Review the menu in advance: Almost all restaurants post menus online, so take the time to review the menu to see what options are listed as gluten-free or “gluten-free optional.” Use this information to evaluate your options and come up with any questions you may have about how the different items are prepared. In general, items that are naturally gluten-free (in other words, don’t have gluten-containing items in them to begin with) are safer than “gluten-free optional” foods (items that have to be modified to be gluten-free), since the modification provides one more step for cross-contamination to occur.
- Call the restaurant ahead: Before dining at a restaurant, give them a call during off-peak hours (for example, mid-afternoon between the lunch and dinner rush) and ask them questions about how they prepare gluten-free items. For example: Do they have a dedicated gluten-free section of their kitchen? Do they clean utensils and serving areas between preparing meals? Are their staff trained in managing allergens? Do they verify that ingredients have not changed when switching suppliers?
- Survey the server: Even if you called ahead, confirm what you learned when you spoke with the cook, chef, or host by talking with the server. For example “I understand you do not have a dedicated gluten-free grill, but that you are able to clean it before preparing my grilled chicken, is that correct? I don’t mind waiting a bit longer for my food as I understand that may take some time, I appreciate the extra care you are taking.”
- Avoid fryers: It is wise to avoid fried food for a number of health reasons, and gluten cross contamination is yet another. Deep fryers are generally used to fry both gluten-containing and gluten-free foods.
- Avoid buffets: Buffets are a cross-contamination nightmare. Even if you know some of the items are gluten-free, you’re relying on all of the people in front of you to use the correct utensils to scoop out food, and to not touch any other food on their plate while they are going through a line. Of course, there is also still the risk of contamination in the kitchen or by an employee, but buffets have the added risk of all of the other guests that may contaminate your food. If you go to an event or wedding with a buffet, call ahead to explain your needs and ask the same questions you would ask of a restaurant, and ask that your plate be prepared in advance and served separately so that you do not have to go through the buffet line.
- Acknowledge extra efforts: If a server or restaurant goes above and beyond to help make you feel safe and cared for, it’s always nice to show gratitude both verbally and through a generous tip. Acknowledging behavior that you appreciate helps encourage it to continue.
Conclusion
Cross contamination is a serious concern for people with celiac disease and gluten intolerance. Not only can it cause an unpleasant short term reaction, it can cause longer term intestinal damage.
The risks of cross contamination can make purchasing packaged foods and dining outside the home stressful. However, knowing how and when food can be contaminated, and preparing certain preparations can help mitigate some of the risks.
I hope this information and these tips are helpful and empowering. Remember, your health is invaluable. Do not ever feel bad advocating for yourself and your health by asking questions and requesting extra accommodations. And finally, remember that healthy whole foods are always a safe bet!


2 Responses
Very good advice . Thanks
Difficult issue for sure as I repeated to my gastrointerologist.
He knows that my antibody test shows baseline levels of inflammation that might be an indicative of some gluten intake and affecting the small intestine of some gluten intake and affecting the small intestine. Before the testing in 2020 I was not gluten free complying for probably almost a year and a One year so I accepted the fact he said there’s border iine information. I advised him I listened to the advice of your nurse to try to be as gluten free as possible at and again mentioned cross contamination possiblely end of story. He didn’t really say anything about that. Today after endoscopic he says you’re intestine looks normal but I took biospy just makes sure there’s no cellular changes But that’s because of some other as well like reflux indigestion. Then at the end of the test when he came to tell me some of the basic results he said did you of course stay on a gluten diet prior to the endescopic exam. Response no your nurse advised me to keep on a gluten free diet knowing the test was 4th coming. Oh well if I had you on gluten for a couple of weeks before will be able to better see changes.. I was confused about the whole remark and he was rush. And I said oh OK well you have poor communication from your staff I guess was my response! When I brought up the cross contamination I said doc you told me I had borderline level before the endo scopic when I was eating gluten non gluten more restricted I still have borderline inflammatory antibodies so clearly mush be cross contamination I suppose. Maybe didn’t he said well you also have some gas strides that I found that you showed me the legion probably possibly from taking Saint John’s war that’s mixing with something else in your routine routine check with your pharmacist. I wasn’t even related to gluten related issues. Is there anything the nurse told me from blood tests they did that I had too much Beta carotene and not enough vitamin E and I take supplements that have the right amounts of adequate of all those vitamins vitamins so they recommended that go see a nutritionist. Unfortunately it’s not covered by my insurance and I’m not even confident with the healthcare system that offers that service because no pait’s obvious because of past experiences with other clinicians they may not be gluten friendly. So the thing is it is what it is you gotta die or something. It was I’m pretty healthy for 71.
.