Protein Deficiency: Why It’s Common in Those With Celiac Disease & Gluten Sensitivity (and what to do about it)
Protein is a hot topic when it comes to food. It often gets associated with high level athletes or praised by those looking to lose weight. On the other end of the spectrum, it often gets vilified by some who advocate for strict plant-based diets.
But the reality is, protein is absolutely essential for human health, and it is estimated that a large portion of the population are deficient. In fact, The Food and Agriculture Organization of the United Nations estimated that approximately one billion people worldwide have inadequate protein intake which contributes to impaired growth and suboptimal health.
That estimate might seem high, given that it includes approximately one-seventh of the world’s population, but actually, it is likely understated. As we will discuss, new research is showing that the benchmarks on which these estimates are based – recommended daily intakes or dietary reference intakes established by government organizations – are set far too low for most individuals.
The truth is, protein deficiency isn’t a condition confined only to third world countries. It is becoming increasingly common among the general population. This is due in part to an increase in processed, nutrient-devoid food that consists primarily of refined carbohydrates and fills a large portion of calories for the day. But it is also due to an increase in certain disease conditions that impair the body’s ability to absorb protein.
This post will dive into all things protein including – what is it, why do you need it, what happens if you don’t get enough, why might you not be absorbing it properly, and how much do you really need?
What is Protein and Why Do We Need It?
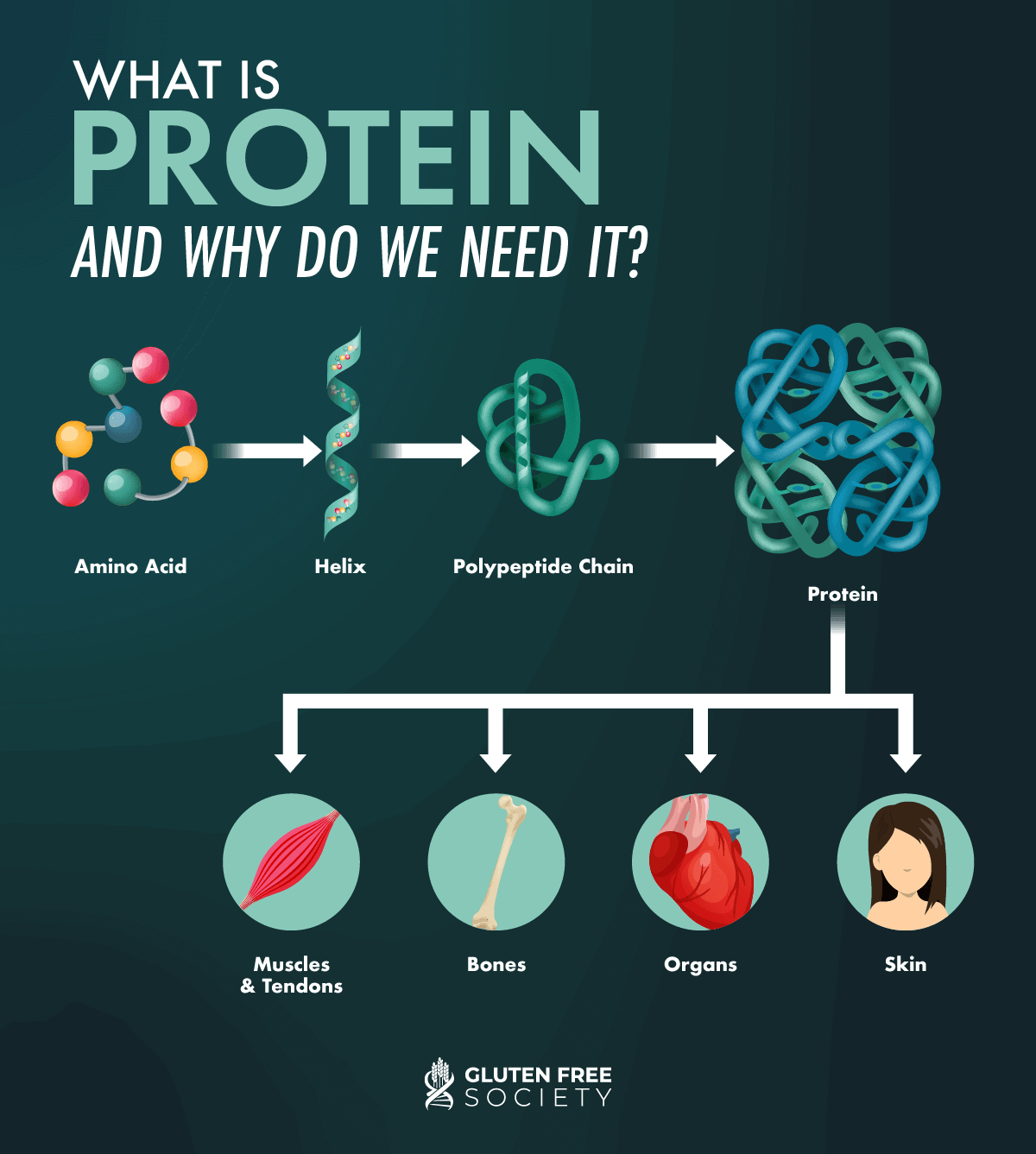
Proteins are the main building blocks of your body. Protein is used to make muscles, tendons, bones, organs, and skin, as well as enzymes, hormones, neurotransmitters, and various molecules that serve many important functions. In other words, protein is involved in the healthy functioning of every organ and system in your body!
Proteins consist of smaller molecules called amino acids which link together to form long protein chains and then fold into complex shapes. When you eat protein, it is broken down into amino acids, which are then used to help your body with various processes such as building muscle and regulating immune function.
Your body can produce some of these amino acids on its own, but others, known as “essential” amino acids, must be obtained through the food you eat. There are 20 total amino acids, and 10 are considered essential: arginine, histidine, isoleucine, leucine, lysine, methionine, phenylalanine, threonine, tryptophan and valine. Generally, the best food sources containing all 10 essential amino acids are animal products.
Signs and Symptoms of Protein Deficiency
As protein is so abundant throughout your entire body, protein deficiency can affect almost all aspects of body function. Therefore, symptoms of protein deficiency are broad and widespread. The following are a few key signs and symptoms of protein deficiency. Note, these are the common symptoms that present early on with a mild or moderate deficiency. Severe protein deficiency comes with more severe symptoms, like edema (swelling) and fatty liver disease.
Your skeletal muscles act as your body’s largest storage vessel for protein. When intake of dietary protein is lower than needed, the body can pull protein from muscles and redistribute it to other tissues and body functions. It’s an adaptive survival tactic that your body has, but unfortunately, it can result in muscle wasting over time if protein needs are not met through the diet. Muscle loss is particularly common in the elderly who are already at a higher risk for muscle loss because of lowered digestive function.
You might not think of bones when you think of protein, but insufficient protein intake has been linked to a lower bone mineral density and an increased risk of fractures. In fact, one study in postmenopausal women with recent hip fractures showed that taking 20 grams of protein supplements per day for 6 months slowed bone loss by 2.3%. The women studied who supplemented with protein also had a shortened rehabilitation time.
- Hair, skin, and nail concerns
Hair, skin, and nails are made primarily of protein. Therefore, thinning hair, hair loss (alopecia), and brittle nails can result from protein deficiency.
While decreased appetite is a symptom of severe protein deficiency, increased appetite is a symptom of mild protein deficiency. When protein intake is insufficient to meet your body’s needs, even in the short term, your body attempts to restore your protein status by signaling that it needs more and increasing your feelings of hunger.
Unfortunately, when our bodies signal hunger, many people reach for quick and easy sources of calories in the form of carbohydrates, not protein. The cycle of insufficient protein intake may lead to weight gain and obesity, an idea known as the protein leverage hypothesis.
Some research has also suggested that protein intake can alter levels of ghrelin, one of your two “hunger hormones.” While the other hunger hormone, leptin, suppresses appetite, ghrelin increases it.
Protein deficiency can negatively impact your immune system. Research suggests this is likely due to the fact that protein contains important amino acids that support your natural immune response. Protein deficiency reduces concentrations of amino acids in the blood. Compromised immunity may mean you get sick more often or that you have a more intense or prolonged illness.
Research has shown that the amino acids in protein are essential for the activation of multiple types of immune cells including – T lymphocytes, B lymphocytes, natural killer cells and macrophages. Additionally, protein plays a role in the maturation and proliferation of immune cells, the production of antibodies, and the production of cytokines (chemicals that regulate inflammation and immune response. Over the last several decades, emerging research in both animal and human studies is showing that dietary supplementation of protein and specific amino acids enhances the immune status, protecting people from the potential of death and disability from infectious diseases.
- Stunted growth (in children)
Protein not only supports the maintenance of muscle and bone mass, it’s also essential for overall growth and development, particularly in children and adolescents. Stunted growth or falling behind on growth charts can be a sign of protein deficiency. The underlying cause may be an undiagnosed disease or food intolerance, or may be due to selective eating as can be common in young children.
How Celiac Disease or Gluten Sensitivity Can Lead to Protein Deficiency
When gluten sensitivity or celiac disease is unmanaged or undiagnosed, deficiencies of macro- and micronutrients can occur. This is generally due to impaired digestion throughout the small and large intestine.
Protein is among the nutrients affected by malabsorption in celiac disease. Malabsorption of dietary protein leads to a deficiency of proteins within the body that can cascade into a number of issues in the body as discussed previously.
Research studies have identified that those newly diagnosed with celiac disease commonly have protein deficiency. When protein deficiency is combined with chronic inflammation as is common in those with gluten induced damage, a vicious cycle can occur. Especially when gluten contributes to damage of the muscles, joints, and tendons. This cycle, commonly referred to as the “Gluten Muscle Wasting Cycle” or the “Grainflammation Cycle” is laid out below.
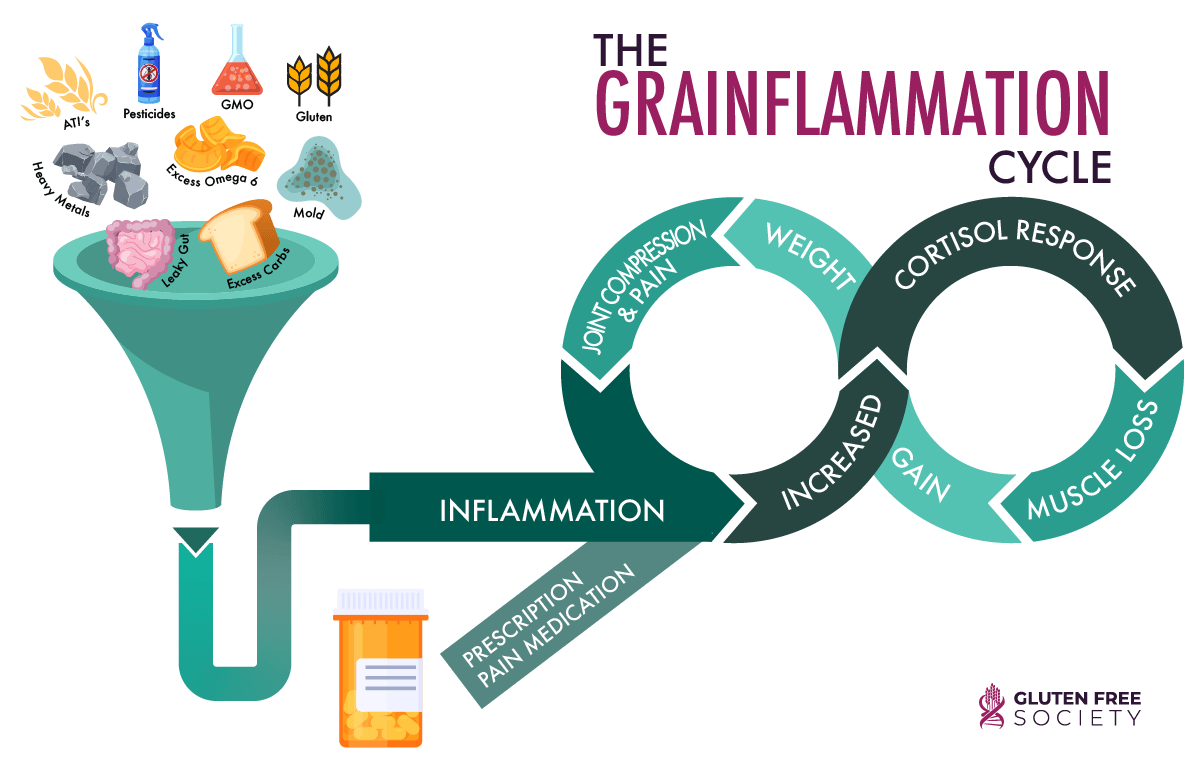
Furthermore, many undiagnosed celiac disease or gluten sensitive individuals learn to rely on acid blocking medication to reduce or manage their confusing and disruptive digestive symptoms. These medications reduce stomach acid and further impair protein digestion.
How Much Protein Should Those with Gluten Sensitivity Be Eating?
A common and logical question to ask (whether or not you are gluten sensitive) is how much protein do I need? The answer is certainly not one size fits all. Like many things related to health, your own personal need depends on a number of factors:
Many nutrition scientists argue that body weight is the most important determinant of protein requirements. For this reason, you’ll typically see protein recommendations presented as grams for each pound or kilogram of body weight.
The recommended daily allowance (RDA) is 0.4 grams of protein for each pound of body weight (0.8 grams per kg). This translates to about 66 grams of protein per day for an adult weighing 165 pounds (75 kg). This might look like 2 eggs for breakfast, 3 ounces of salmon for lunch, and 4 ounces of chicken breast for dinner (alongside plenty of fresh veggies, nuts, seeds, and other whole food sources of micronutrients, healthy fats, and fiber, of course).
However, a growing body of research suggests this range is understated. In fact, current evidence indicates that intakes in the range of at least 1.2 to 1.6 grams per kilogram per day of high-quality protein is a more ideal target for achieving optimal health outcomes in adults.
Weight can be used as a baseline to indicate the minimum amount of protein your body needs. The following factors can layer additional needs on top of this baseline.
Health status can mean many things, from body composition to underlying disease conditions, and each of these can impact protein needs.
For example, having a higher muscle mass increases your need for protein. This is because protein is necessary to maintain higher levels of muscle. Without sufficient protein at any level of muscle, the muscle cannot be maintained and will “waste” or break down.
In addition, protein intake can help the management of many disease conditions, like type II diabetes. Research has shown that dietary protein and amino acid metabolism may be leveraged to optimize glycemic regulations. Therefore, protein intake, particularly in relation to carbohydrate intake, can benefit those with compromised blood sugar management and diabetes.
Protein requirements are also higher in those with chronic and/or systemic inflammation. This may be driven by a number of disease conditions, including food intolerances and allergies. Chronic inflammation causes unavoidable protein catabolism even if eating a diet that is optimal in meeting nutrition needs. One study suggests that in a state of chronic and/or systemic inflammation, “a relatively high protein intake may be required to promote synthesis of specific proteins, prevent depletion of selected amino acids (e.g., glutamine or arginine), modulate immune functions, and counteract insulin resistance and redox imbalance. Thus, an optimal protein/amino acid intake may be greater than that required to decrease whole body protein wasting.” Those with undiagnosed or recently diagnosed celiac disease or gluten sensitivity often have high levels of inflammation in the body that will raise protein requirements.
- Physical activity frequency and intensity
Physical activity causes your body to break down muscle fibers. In order to rebuild and restore muscles, your body requires additional protein – above and beyond your baseline requirements.
While The American College of Sports Medicine recommends a daily protein intake ranging from 1.2–1.4 grams per kilogram (0.5 to 0.6 grams for each pound of body weight), many scientists and other sports organizations believe this is too low.
The International Society of Sports Nutrition’s daily recommendation is 2 grams per kilogram (0.9 grams of protein per pound of body weight) for athletes. This higher recommendation is more in line with other emerging research on higher protein needs for all populations.
Like athletes, older adults seem to have higher protein requirements. In fact, one small study estimated that recommendations for adults aged 65+ were underestimated by approximately 30%, with a suggested target of 0.94 grams to 1.24 grams per kilogram of body weight per day. Another review of research concluded that there is “good consistent evidence that consumption of 1.0 to 1.3 grams per kilograms per day of dietary protein combined with twice-weekly progressive resistance exercise reduces age-related muscle mass loss.”
A large-scale study, the PROT-AGE study, concluded that an optimal range for the 65+ population is between 1.0 to 1.2 grams per kilogram of body weight per day. The study also considered our prior two discussion points: health status and physical activity. The study recommended a higher protein intake of (greater than 1.2 grams per kilogram of body weight per day) for those who are exercising and otherwise active, and a higher intake (1.2-1.5 grams per kilogram of body weight per day) for older adults who have acute or chronic diseases.
As we mentioned, proteins are the main building blocks of the body – they are needed to maintain and build every cell in your body. And as you might imagine, there are a lot of new cells being created during pregnancy. That means that more protein is needed to support a pregnant woman’s body (her own changing organs and tissues and increased blood volume) and her growing baby.
But how much more does a pregnant woman need? Again, recent research indicates that needs are higher than guidelines suggest. It’s important to note that recommendations were set using estimates for nonpregnant males and females, estimating an increase from a baseline. The first ever study to directly measure protein needs in pregnant women found that true protein needs were 39% higher in early pregnancy and 73% higher in late pregnancy compared to the estimated average requirement (EAR). The study suggested the EAR should be set at 1.22 grams per kilogram in early pregnancy and 1.52 grams per kilogram in late pregnancy.
Protein quality and supplementation
For some people, particularly those with higher needs, it isn’t feasible to obtain adequate protein from diet alone. However, the quality of protein supplements on the market varies widely. Many are filled with additives – including sugar, artificial colors and flavors, and gut-damaging gums and fillers. If you believe a protein supplement would benefit you, I recommend seeking out a high-quality animal-based option, like grass-fed beef bone broth protein or collagen peptides. Plant-based proteins often contain other inflammation-promoting grains like rice or GMO corn-based fillers. If you opt for plant-based protein, be sure to seek out a clean formula without these detrimental ingredients. Note that plant-based proteins can also be high in heavy metals, pesticides, and mycotoxins (especially those containing grain-based protein), so be sure to purchase from a reputable brand that you trust.
Conclusion
Protein is a critical macronutrient that supplies important amino acids to nearly every organ and system in the body. Protein deficiency is common and needs are higher than many mainstream recommendations tend to suggest. Needs are especially higher for those with gluten sensitivity, celiac disease, and other chronic inflammatory health conditions, as well as older adults and active individuals.
If you are wondering if you are getting enough protein, start by logging your intake of protein each day for a week, then compare it to your body weight to get a baseline of what you currently consume. Consider your own personal age, activity level, and health status to understand whether or not you may be falling short. Try increasing your daily intake as needed through high quality food sources of protein and observe any changes in your physical and emotional health. Of course, if you feel you need more personalized attention, seek the help of a qualified provider who can help you navigate your individual needs.
12 Responses
My phone died during ur video on protein deficiency. I am having severe problems with corn. I noticed that threonine is a hidden source of corn. Is threonine in collagen peptides made from corn?
Depends on the source of collagen peptides. Corn is not typically used if collagen is derived from animal sources.
Im curious, if a general problem with protein digestion and absorbtion in yhe intestines is related to long term undiagnosed celiac disease, why recommend increased protein intake rather than enzymes? Also, are there some proteins that are more challenging to digest? Where can i find your sources for this article? I would like to read more about the topic. Thanks!
Hi Alyx,
Gluten can damage the small intestine, liver, and pancreas. This damage can cause maldigestion/absorption issues. The most important solution is to remove gluten from the diet. Digestive enzymes can be taken for support, but real healing happens with the diet change. All of the blue text in the article are links to research studies and sources.
Have a great day!
Dr. O
I know I am Coeliac. Handed down generations. I do my best to eat as much protein as possible..
Protein gives me really bad constipation. Is there an easier form of Protein that I can take?
Chris you might try 2 things:
1. Ultra Acid – This supplement will support your ability to properly digest protein.
2. Warrior protein – this is an organic plant based protein that is easy to digest.
This is fascinating! I noticed the palms of my hands get red and blotchy from time to time and all I could find was Palmar Erythema (which is what it looked like exactly) and liver cirrhosis. But I don’t have that. Then I found very old scientific papers based in the 1940s or earlier that stated they noticed this phenomenon when n some remote countries or villages where protein wasn’t eaten enough and once they increased their protein intake it resolved. So low and behold I increased my animal protein intake, because it seems I don’t absorb plant protein well at all, which is what landed me to have these symptoms in the first place, and sure enough my symptoms resolved completely upon increasing my animal protein intake. It’s frustrating though because I would like to be more plant based but for some reason, probably the gluten intake most of my life (resulting in damage) has prevented me to do so.
Thank you for this. I have not been able to find many current blogs or content on the relation between celiac/gluten and protein deficiency
Kind of curious as to why many (some do) don’t calculate protein requirements based on lean body mass rather than total weight. LBM is where we need the protein, not adipose tissue. Just sayin’. Any thoughts? Thanks.
Just What I Needed To Read About Protein!!! 3/17/2022 I Received An Ileostomy – Surgery Went Well & I Love My “Jilly”!!! I’ve Been Gluten,etc., Free Since 1995!!! Before My Surgery, I Had To Build Up To 120 lbs. To Have The Operation – My Diseased Colon Removed Weighed 25 lbs. Not To Say The Least, I Had Major Serious Colon & Rectum Problems – I Came Home At 87 lbs. & Stayed That Way For 8 months!!! My Food Sensitivities Are Off The Charts – I Just Recently Gained 7 lbs. By Adding Quite A Bit Of Almond (SAFE) Cheese – It’s All Almond!! I Don’t Know If I’m Overdoing It Because I Gain A Pound A Week – So Fast!!! I’m 66 yrs. old, 5 Feet, 93 lbs. – Goal Is 95 lbs – I Forgot To Mention That I Only Eat 10 Different Foods- OCD, Depression, Anxiety, MAJOR MIGRAINES, My Recent Thyroid Results (AND I’VE HAD HYPOTHYROIDISM FOR 35 yrs.) Came Back Extremely Lower Than The Low I Already Have. Dr. Doesn’t Feel We Should Increase My Synthroid So I Did It Myself!!! That May Seem Crazy But Because My Hot Flashes Returned 3 mnths. (I WENT THROUGH MENAPAUSE IN MY EARLY 50’S), MIGRAINES ON A RISE AT A RAPID PACE, & OTHER SYMPTOMS HAVE SURFACED!!! I DID A DESPERATE MOVE BUT I FEEL A SHIFT – GOING TO GET KETAMINE TREATMENTS FOR MEDICATION RESISTANT DEPRESSION (ALMOST 40 yrs. – NO DRUG WORKED – Went All Through Trudy Scott’s Amino’s – No Luck!!! I’M USING CBD FOR ANXIETY LATELY – BUT THAT HELPS ANXIETY NOT DEPRESSION – ANY HELP & ADVICE FROM YOU WOULD BE GREATLY APPRECIATED – I Forgot – I Eat Eggs & Chicken – All Ingredients AOK!!! I’VE BEEN FOLLOWING ALL OF YOUR WORK FOR A LONG TIME!!!! PLEASE HELP – SOS!!!!
Hi Gluten Free Society,
My name is Scott. I was diagnosed Celiac in 2008, I was 35 then. I was diagnosed with the blood test and via a sample taken from my intestine which confirmed the diagnosis and indicated an approx 40% loss or score of 2 out of 5 for intestine damage. I also had a liver ultrasound done that indicated my liver was much larger than it shuold be. I don’t consume alcohol. I also had a bone density test that confirmed Osteopenia and I recently had a protien absorbtion test done for the first time which indicated low protien levels which was a surprise since I’m consuming high amounts of protien with my regualr food diet and via supplementation. I’m regularly feeling inflammed with tight joints. So with all that informaiton in mind my quesiton is do you know of any highly respected and informed celiac nutritionists that you’d be able to recommend to help me create a diet plan. I think the time has come that I stop trying to figure things out on my own. Thanks in advance.
Scott,
Sorry to hear that you are going through this. You might consider reaching out to Dr. Osborne’s practice – 281-240-2229