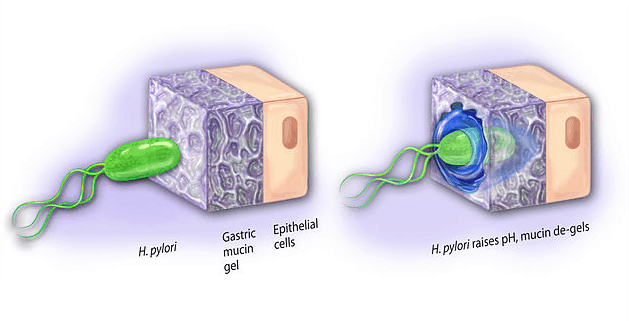
Chronic gluten exposure for those who are intolerant can weaken the immune system’s ability to fight off infection. One of the most common types of infection in the GI tract (stomach) is a bacteria called Helicobacter pylori (AKA- H. pylori). This bacteria can bore through the stomach mucus and cause erosion of the lining in the stomach and duodenum leading to ulcers. If the infection persists long enough it can contribute to dysplastic cell growth and stomach cancer. Common symptoms of H. pylori infection are:
- Gastric bloating
- Heartburn or acid reflux
- Nausea
- Black tarry stools
- Excessive belching
- Vomiting
- Loss of appetite
A new research study has discovered another potentially dangerous symptom linked to H. pylori infection –
Iron Deficiency Anemia. Adults with the infection as well as persistent iron deficiency were treated. After the bacteria was eradicated, iron deficiency corrected in 38% of the patients being treated (iron levels corrected without supplementation).
This study is important because many patients with a history of gluten sensitivity have refractory iron deficiency. Refractory means that their anemia does not correct with iron supplementation. In these patients, H. pylori infection should be ruled out as a contributing factor. If discovered a treatment regimen against the infection should be implemented while iron levels are monitored. For symptoms and problems linked to
iron deficiency go here <<<
Source: World J Gastroenterol. 2013 Jul 14;19(26):4166-71. Helicobacter pylori infection as a cause of iron deficiency anemia of unknown origin.
The Problem With Traditional H. pylori Treatments
Most doctors prescribe triple therapy – a combination of proton pump inhibitors (PPI’s), clarithromycin, and amoxicillin. This combination of acid blocking and antibiotics has become less and less effective due to antibiotic resistant strains of H. pylori. Additionally, many patients have severe adverse reactions to this therapy – the symptoms of which can be worse than the infection.
Natural Support for H. pylori Control
There are many natural botanicals that have been studied and shown to be effective at destroying H. pylori. Because of antibiotic resistance, these botanicals are often times better options. You should talk with a functional medicine doctor more about this avenue. Common botanicals used for H. pylori include – mastic gum and berberine. Additionally, a number of healthy foods have anti-bacterial effects including garlic, onion, oregano, thyme, and coconut. Liberal use of these foods can be considered in addition to botanicals for those wanting to implement food based support.
Bottom Line
If you have chronic iron deficiency even after supplementing appropriately with iron, you should consider having your doctor rule out an H. pylori infection. If present, I recommend taking a regimen of the following:
The above regimen can be taken safely for several months without side effects. If you start feeling better, never assume that the infection is cleared up. H. pylori can be insidious, and much like gluten, it can cause damage without outward symptoms. Always ask your doctor to run the appropriate lab tests to ensure eradication of the bacteria after treatment protocols are complete.
Always looking out for you,
Dr. O – The Gluten Free Warrior
11 Responses
Definitely I believe their is a connection to gluten and H pylori and anemia. I myself years ago before being diagnosed Celiac and then with H Pylori have spend many years since studying this factor. Absoluely always rule out gluten.
I had a blood test that showed no h pylori antibodies. I still think I have SIBO or candida, something’s going on. What’s weird is that when I started drinking a huge glass of lemon water and blackstrap molasses in the morning my IBS issues have subsided that I’ve had since a bad glutening in October 2013. I have celiac disease as well. Oh and I have also been taking between 50-100 billion probiotic cultures a day. Started doing this about a week ago and IBS issues are very improved. Just don’t know why?
Need to check with any anemia and chronic iron deficiency–you may have Beta Thalassemia Major (or Minor).
Could there be a correlation between H-pylori and too much iron (hemochromatosis)? I am under the impression that iron feeds bad bacteria which seems to be the opposite of what your article talks about
Hi Margie,
Iron deficiency can increase the risk for infection, as well, iron excess can help feed an infection.
Iron supplementation is typically best done with appropriate monitoring of iron levels to prevent a problem.
You might find this article educational-
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3856365/
All the best,
Dr. Osborne
My stomach gurgles most of the time after eating or drinking & I seem to have hunger pains often since I’m not eating very much at once! If I eat a larger amount, I feels heavy inside like I’ve eaten bricks! So sick of this! Had a tragedy in my life a few months ago @ my stomach seems tone where this stress has hit me!
I was taking Omeprazole daily for really awful heartburn and GERD as a teenager and hadn’t yet been diagnosed with helicabacta bacteria when I moved to the Middle East to study. The locals didn’t eat any leavened bread and I didn’t like flat bread so I stopped eating as much gluten as I did at home without thinking about it and my heartburn and asthma greatly improved! When I returned home the symptoms came back and I ended up stupidly taking anti biotics. I was only 20 at that time and didn’t know anything about gluten. Definitely a link !!
Hi Claire,
Same problem is with can you just advise me, did you find relief from this problem.If yes can you please also advise how did you get ??
Hi
I have just come out of surgery from peptic ulcer. Always did suspect h pylori just from my own research. As im due to go for my post op check up in 2 weeks would there be any way i could contact Dr. Osborne to discuss natural remedies etc…
Could anyone please let me know how i can get in contact.
Thank you kindly
i am 23 years old and since May 2018. it was discovered that I was anemic . The doctor reccommended 9 iron infusions which pumped my hemoglbin from 7.8 to 11. Then I was prescribed iron supplements until December which increased my hemoglobin levels to 13.4 but my ferritin was at 3. The doctor prescribed Sideral Forte iron supplement. In Janunary of 2019 I was feeling drowsey and brain fog so I went to different which ferritin test showed a level 5. Hemoglobin rising to 14, the doctor checked for other nutritional deficiencies but none were found. I did a TTG IGG test which stated coeliac disease. Endoscopy was conducted which was not comclusive of coeliac . Since March I am on gluten free diet. i had infection mid march where antibiotics was prescribed.While having the medicine , i did not have brain fog and blood from my gums had decreased during those 20 days . Then again brain fog and fatigue started again . My ferritin in march stood at 12 and doctor afvised 5 iron infusions. For some reason I had an infection and 3 injections of iron were given each of 1.5 mg. I am sceptical that i am HPylori positive rather than coeliac , cause there was no pain on gluten encounter before.
I was fine eating gluten food prior to have H Pylori. A month after diagnosing H Pylori, i started to feel iron deficiency anemia symptoms and it ended up I have it. Then tested for food sensitivities and discovered I developed gluten sensitivity as know as non celiac. For me H Pylori caused it all…